To evaluate exercise capacity using the 6-minute walk test (6MWT) in patients with complicated silicosis, and to determine how results shape the prognostic value of 6MWT for hospitalization and mortality.
MethodProspective observational study in 143 patients with complicated silicosis who performed the 6MWT in our outpatient pulmonology clinic between 2009 and the end of 2016. Lung function tests, computed tomography findings and 6MWT parameters (distance walked and oxygen desaturation) were evaluated.
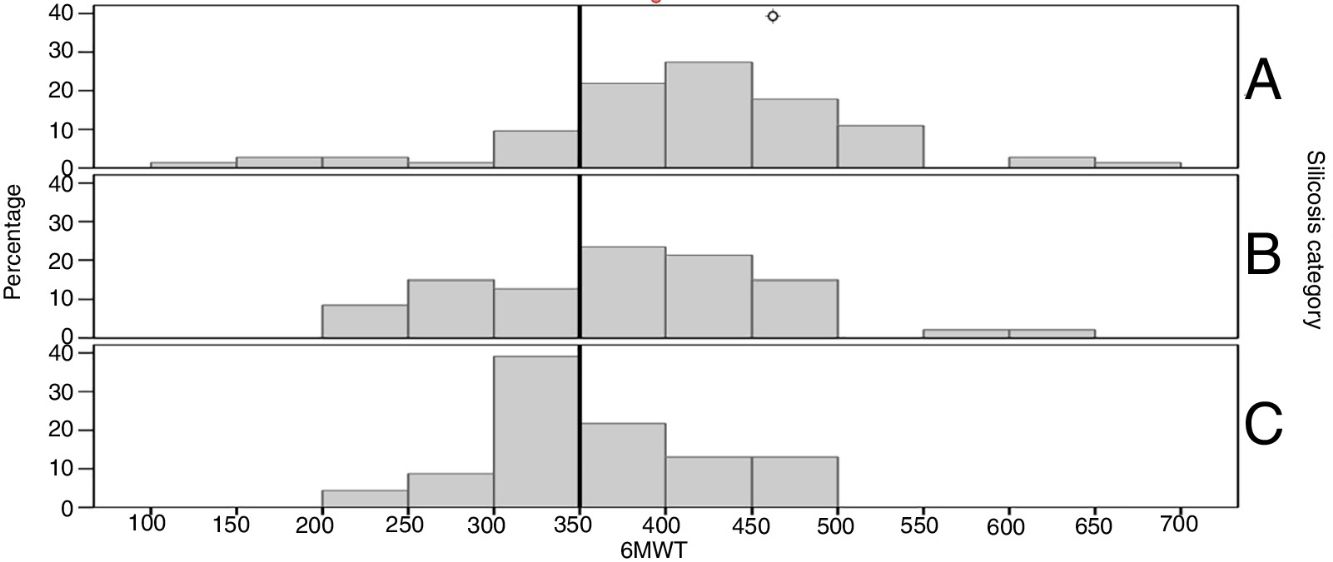
ResultsPatients with complicated silicosis walked 387±92m. Results deteriorated as silicosis severity increased; category A: 407±97m, B: 370±88m, and C: 357±68m (P=.022). The 6MWT correlated positively with lung function and inversely with dyspnea determined by mMRC (P<.001). Patients with moderate/severe emphysema and greater CT90 presented a worse result on 6MWT. Patients who walked <350m had more hospitalizations (3.7±4.0) than those who walked >350m (1.1±2.9). There was an impact on survival: non-survivors walked 327.9±73.0m, while survivors walked 404.5±89.7m (P<.001).
ConclusionsSpirometry values and category of complicated silicosis correlated with 6MWT and distance walked was a prognostic factor for hospitalization and mortality. The 6MWT is a useful tool in occupational health for monitoring patients with silicosis.
Evaluar la capacidad de ejercicio, utilizando la prueba de la marcha de 6 minutos (6MWT), en pacientes con silicosis complicada, e identificar factores relacionados con dicho resultado, así como su valor pronóstico de hospitalización y mortalidad.
MétodoEstudio observacional prospectivo en 143 pacientes diagnosticados de silicosis complicada atendidos en consulta de neumología desde 2009 hasta diciembre 2016, sin limitación para hacer la 6MWT. Se evaluaron las pruebas de función pulmonar, los hallazgos de la tomografía computarizada y los parámetros de la 6MWT (distancia caminada y desaturación de oxígeno).
ResultadosLos pacientes con silicosis complicada caminaban una media de 387±92m. Los resultados fueron peores al aumentar la gravedad de la enfermedad; en silicosis A: 407±97; B: 370±88, y C: 357±68 (p=0,022). La 6MWT mostraba una correlación positiva con la función pulmonar e inversa con la disnea (p<0,001). Los pacientes con enfisema moderado/severo y un mayor tiempo con saturación nocturna de oxígeno por debajo del 90% presentaban resultados significativamente peores en la 6MWT. Los pacientes que caminaban <350m tenían más hospitalizaciones (3,7±4,0) que los que caminaban >350 (1,1±2,9). Los fallecidos al final del seguimiento caminaron 327,9±73,0 frente a los que sobreviven, que caminaron 404,5±89,7m (p<0,001).
ConclusionesLos valores de la espirometría y la categoría de la silicosis se relacionan con el resultado de la 6MWT, que resultó ser factor pronóstico para hospitalización y mortalidad. La 6MWT se perfila como una herramienta útil en salud ocupacional para el seguimiento de pacientes con silicosis.
Silicosis, one of the most common occupational respiratory diseases in our setting,1 is an irreversible chronic interstitial lung disease caused by protracted inhalation of silica dust in a crystalline form. The annual reports of the National Institute of Silicosis record an increase since 2008 in new diagnoses from industries other than coal mining, such as the granite, slate and artificial silica conglomerate sectors. In 2012, 166 were cases reported by the National Institute of Silicosis, and of these 64 (38%) were from Galicia, and 34 in particular (20%) were from the granite sector, located in the health area of our hospital.2
The 6-minute walk test (6MWT)3 is a test widely used for evaluating exercise capacity by measuring the distance walked in 6 minutes. It is easy and inexpensive to perform, and reflects the functional capacity of patients, proving itself to be useful and reproducible in various respiratory diseases.4,5 Various studies have demonstrated its usefulness in chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis, where it not only helps determine the need for supplemental oxygen, but is also a prognostic indicator for predicting mortality and evaluating the indication of lung transplantation.6,7
The degree of respiratory functional involvement is a fundamental determinant for evaluating incapacity for work and for monitoring the progress of severity in patients with silicosis. These parameters are currently determined from lung function tests, supplemented by clinical criteria. First-line tests for measuring lung function are forced spirometry and diffusion capacity of the lung (DLco), while second-line functional tests include cardiopulmonary exercise testing and lung volumes.8 Given that the correlation between exercise capacity and spirometry results is less than optimal, other assessments, such as exercise testing, are required to determine exercise tolerance in some cases.9 In patients with interstitial lung disease presenting as silicosis, exertion dyspnea, which is incapacitating in many cases, is common and correlates closely with ventilatory limitation shown on the cardiopulmonary exercise test.10 The maximum stress test provides an accurate assessment, but costs in terms of both equipment and human resources are higher than those of a submaximal exercise test, such as the 6MWT. In idiopathic pulmonary fibrosis, dyspnea has been correlated with distance walked on the 6MWT.11 However, the evidence available to recommend the 6MWT in patients with silicosis has been scant until now,12 and the few reports published have been in the form of letters or communications to congresses.13–15 The objective of our study was to evaluate exercise capacity using the 6MWT in patients with complicated silicosis, in order to identify factors associated with the results of this test and to determine its prognostic value by analyzing the relationship of the 6MWT with hospital admissions and mortality.
MethodThis was a prospective study of all silicosis patients seen in a silicosis clinic who performed a 6MWT between 2009 and 2016. The indication for performing the test was altered lung function (forced expiratory volume in 1 second [FEV1]<80% and a FEV1/forced vital capacity [FVC] ratio<70% or FVC<80%), and/or dyspnea (MRC≥1). We excluded studies performed with supplemental oxygen, in order to eliminate the oxygen as a confounding factor in determining the prognostic value of oxygen desaturation. Silicosis was diagnosed in accordance with the guidelines of the Spanish Society of Pulmonology and Thoracic Surgery.12 Simple chronic silicosis was defined as opacities measuring <10mm and complicated chronic silicosis as opacities >10mm. Only patients with complicated silicosis were included in the study.
All patients included had undergone at least 1 computed tomography (CT) scan interpreted by consensus between 2 radiologists with extensive experience in silicosis. Small opacities were classified into 4 categories according to profusion, in a manner similar to that used to classify chest radiographic findings: (0) no small opacities; (1) small numbers of small opacities; (2) abundant small opacities with vascular blurring; (3) very abundant small opacities with poorly visible normal lung anatomical structures.16,17 Large opacities were classified as follows: category A: 1 or more opacities measuring more than 10mm and occupying less than a quarter of the area (1 quadrant) in the right side at the level of the carina on CT; category B: an opacity greater than “A” but occupying less than half of the area (2 quadrants) in the right side at the level of the carina on CT; and category C: when one opacity or the sum of the opacities comprised more than half of the area in the right side at the level of the carina on CT.17 Emphysema was assessed according to subjective criteria and categorized by visual inspection as absent (<5% of affected lung), mild (5–25%), and moderate-to-severe (>50%), similarly to various chronic obstructive pulmonary disease studies.16,18,19 Nocturnal oxygen saturation was assessed with a night-time recording on the same day as the 6MWT was performed, using pulse oximetry (Minolta® Pulsox 3i). CT90 was taken as the time with oxygen saturation less than 90%. Comorbidity was assessed with the Charlson index.20
Lung function tests, spirometry, and determination of DLco were conducted following the recommendations of the Spanish Society of Pulmonology and Thoracic Surgery, and the European Respiratory Society.21,22 The main variables of forced spirometry are FVC and FEV1. FVC represents the maximum volume of air exhaled in a maximal expiratory maneuver, initiated after a maximum inspiration maneuver, expressed in liters. FEV1 corresponds to the maximum volume of air exhaled in the first second of the FVC maneuver, also expressed in liters, while the FEV1/FVC ratio shows the relationship between the 2 parameters. The single breath technique22 was used to determine the diffusing capacity of the lung for carbon monoxide (DLco), and the helium dilution method was used to determine static volumes, including total lung capacity.23 Obstructive airflow limitation was defined as a FEV1/FVC ratio of <70.24 The 6MWT was performed according to the recommendations of the American Thoracic Society,25 along a 30-meter corridor. While resting, the patient received an explanation of what was involved in the test and was told that they should walk as far as possible in 6 minutes without running. Resting blood pressure was determined and dyspnea was measured according to the Borg scale and muscle fatigue according to the modified Borg scale. A pulse oximeter was placed to record oxygen saturation and heart rate throughout the test. During the test, the patient received standardized encouragement using previously protocolized phrases, specified in the American Thoracic Society guidelines.
Oxygen desaturation during the walk test was defined as a reduction in saturation at the end of the test ≥4% and/or if oxygen saturation fell below 90%.
The study was approved by the Research Ethics Committees Network of Galicia (Registry No. 2009/467) and was performed according to the principles of the Declaration of Helsinki and subsequent updates, and prevailing biomedical research legislation.
The statistical analysis included a descriptive and analytical study of the data. The results of qualitative variables were represented as frequency and percentage, and quantitative variables as mean and standard deviation. The main study variables were compared between 2 groups of patients: those who walked more and those who walked less than 350m in the 6MWT. The results of the 6MWT were classified on the basis of the 350m threshold determined from observations from previous studies26,27 and the point that best discriminated complicated grade B and C silicosis from grade A silicosis, obtained from a ROC curve. We used the chi-square test to compare qualitative variables and Student's t-test to compare quantitative variables. A logistic regression analysis was also performed to study which variables were associated with higher mortality in these patients. Differences were considered statistically significant when P was <.05.
ResultsOf the total number of subjects evaluated in the silicosis clinic during the study period from 2009 to 2016, 370 had a diagnosis of silicosis. Of these, 8 had no lung function tests, 77 did not perform the 6MWT because their lung function tests were normal, and 65 with abnormal lung function either could not perform the 6MWT, or performed it but the results could not be analyzed because they were receiving oxygen at the time. Seventy-seven patients had uncomplicated silicosis and 143 had complicated disease.
Of the 143 patients with a diagnosis of complicated silicosis who performed the 6MWT, all were men, with a mean age of 52.6±10.7, grade A silicosis: 73, grade B: 47 and grade C: 23. With regard to their occupational history, 118 (82.5%) worked in quarries, 10 (7.0%) in ornamental stone workshops, 3 (2.1%) in sand and gravel works, and 12 (7.7%) were from other sectors. The mean distance walked by the cohort was 387.9±91.7m; 47 patients (32.9%) walked less than 350m, and 96 (67.1%) walked more than 350m. Mean patient follow-up was 5.1±2.1 years, during which period 31 patients died (21.7%).
The demographic, clinical, and functional characteristics of the study population are shown in Tables 1 and 2. Table 1 shows that the group who walked less than 350m had a greater number of hospitalizations (P<.001) and a higher rate of moderate-severe emphysema; 50% of patients with moderate-severe emphysema walked less than 350m (P<.001), and had greater degree of dyspnea on mMRC (P<.001). Significant differences were found between the different categories of complicated silicosis (A, B, and C). Among patients in the complicated silicosis category A, 58 (79.5%) walked more than 350m, while in category B, only 27 (57.4%) did so, and in category C only 11 (47.8%) patients walked more than 350m (P<.001). Moderate-severe emphysema also correlated with a worse outcome on the 6MWT. Seventy-five patients with complicated silicosis (52.4%) had obstructive airflow limitation. Table 2 shows that patients in the group who walked less than 350m showed worse lung function results in all parameters studied, except in FVC and total lung capacity.
Characteristics of Patients According to Distance Walked in the Six-Minute Walk Test.
| 6MWT | P | ||
|---|---|---|---|
| <350m (n=47) | >350m (n=96) | ||
| Age (mean±SD) | 57.8±11.7 | 50.1±9.2 | <.001 |
| Complicated category; n (%) | |||
| A | 15 (20.5) | 58 (79.5) | .004 |
| B | 20 (42.6) | 27 (57.4) | |
| C | 12 (52.2) | 11 (47.8) | |
| Smoking habit (PYI); mean (SD) | 27.1±17.7 | 24.7±17.5 | .530 |
| BMI; mean±SD | 26.9±3.5 | 26.8±3.7 | .848 |
| Hospitalizations; mean±SD | 3.7±4.0 | 1.1±2.9 | <.001 |
| Emphysema; n (%) | |||
| No/mild | 24 (24.7) | 73 (75.3) | .003 |
| Moderate/severe | 22 (50.0) | 22 (50.0) | |
| MRC; n (%) | |||
| 0 | 3 (15.0) | 17 (85) | <.001 |
| 1 | 10 (17.2) | 48 (82.8) | |
| 2 | 18 (41.9) | 25 (58.1) | |
| 3 | 13 (68.4) | 6 (31.6) | |
| 4 | 2 (100.0) | 0 (0.0) | |
| Charlson index; mean±SD | 1.3±1.6 | 0.9±1.3 | .392 |
| CT90 (%); mean±SD | 25.7±32.1 | 11.3±20.2 | .012 |
| Desaturation<4%; n (%) | 21 (44.7) | 17 (17.9) | .001 |
| Saturation<90%; n (%) | 13 (27.7) | 13 (13.7) | .043 |
| Profusion; n (%) | |||
| Category 1 | 3 (37.5) | 5 (62.5) | .428 |
| Category 2 | 21 (28.0) | 54 (72.0) | |
| Category 3 | 23 (38.3) | 37 (61.7) | |
Lung Function Results in Both 6MWT Groups.
| 6MWT | P | ||
|---|---|---|---|
| <350m n=47 | >350m (n=96) | ||
| FVC, l; mean±SD | 2.838±907 | 3.745±3.142 | .084 |
| FVC (% predicted); mean±SD | 66.7±17.8 | 73.8±15.6 | .017 |
| FEV1, l; mean±SD | 1.762±854 | 2.405±708 | <.001 |
| FEV1 (% predicted); mean±SD | 55.1±22.2 | 68.3±18.2 | .001 |
| FEV1/FVC ratio (%); mean±SD | 60.6±16.4 | 69.7±11.2 | .001 |
| TLC (% predicted); mean±SD | 72.1±16.3 | 76.6±13.6 | .118 |
| DLco (% predicted); mean±SD | 60.3±21.3 | 71.7±16.4 | .001 |
Thirty-one (21.7%) of the 143 patients died, 20 (64.5%) from respiratory causes, 3 (9.7%) due to non-respiratory cancer, 1 (3.2%) due to cardiovascular disease, and 7 (22.6%) from other causes. Table 3 shows the results of demographic, clinical and lung function variables of patients who died during follow-up. Some of the variables were significantly associated with mortality. A multivariate analysis was performed with the variables that were significant in Table 3, and revealed that an oxygen saturation of less than 90% at the end of the test (OR 5.3; CI 95% 1.7–16.5; P=.004), less than 350m walked on the 6MWT (OR 3.2; CI 95% 1.1–9.6; P=.033), silicosis category B (OR 4.6; CI 95% 1.3–16.7; P=.019), silicosis category C (OR 4.2; CI 95% 1.0–17.9, P=.050), and older age (OR 1.07; CI 95% 1.02–1.13; P=.004) are associated with a greater probability of death.
Classification of Patients According to Survival During Follow-Up.
| Variables | Death | P | |
|---|---|---|---|
| No (n=112) | Yes (n=31) | ||
| Age; mean±SD | 50.3±8.9 | 60.9±12.4 | <.001 |
| Complicated category; n (%) | |||
| A | 68 (93.2) | 5 (6.8) | <.001 |
| B | 30 (63.8) | 17 (36.2) | |
| C | 14 (60.9) | 9 (39.1) | |
| Smoking habit (PYI); mean±SD | 22±0.9 | 24±0.9 | .176 |
| BMI; mean±SD | 26.7±3.8 | 27.0±2.9 | .717 |
| Charlson index; mean±SD | 0.9±1.3 | 1.5±1.6 | .614 |
| FVC, l; mean±SD | 3,688±2.972 | 2.633±692 | .075 |
| FVC, % predicted; mean±SD | 73.9±16.1 | 63.1±15.9 | .001 |
| FEV1, l, mean±SD | 2.402±754 | 1.477±555 | <.001 |
| FEV1, % predicted; mean±SD | 68.2±19.5 | 49.1±17.0 | <.001 |
| Desaturation ≥4%; n (%) | |||
| Yes | 20 (52.6) | 18 (47.4) | <.001 |
| No | 91 (87.5) | 13 (12.5) | |
| Decrease to <90%; n (%) | |||
| Yes | 11 (42.3) | 15 (57.7) | <.001 |
| No | 100 (86.2) | 16 (13.8) | |
| Emphysema; n (%) | |||
| No/mild | 85 (87.6) | 12 (12.4) | <.001 |
| Moderate/severe | 26 (59.1) | 18 (40.9) | |
| 6MWT, m; mean±SD | 404.5±89.7 | 327.9±73.0 | <.001 |
| Profusion; n (%) | |||
| Category 1 | 6 (75.0) | 2 (25) | .097 |
| Category 2 | 64 (85.3) | 11 (14.7) | |
| Category 3 | 42 (70.0) | 18 (30.0) | |
This study analyzes for the first time the results of the 6MWT conducted in patients with silicosis. We found that the results of this test are often abnormal in this group of patients. Factors such as the presence of complicated silicosis grade B or C, moderate or severe emphysema, alterations in lung function, and desaturation during the test and during the nocturnal oximetry recording contribute to a worse outcome in the 6MWT and a worse prognosis in terms of readmission and death. This study reveals a close correlation between the 6MWT results and lung function and degree of dyspnea on MRC. We observed that most lung function parameters analyzed correlated significantly with the results of the 6MWT. Favre et al.28 reported a series of 38 ex-miners, in which patients with altered lung function tended to walk a shorter distance. In our series, the distance walked decreased in line with increasing severity of the disease. In contrast, Cozza et al., in a communication to the European Respiratory Society published as an abstract in 2013,13 reported a series of 67 patients (with the same percentage of obstructive lung disease as ours, 49%) in which they found a correlation with lung function but not with the severity of radiological opacities. Similarly, Noh,14 in a letter to the editor, published a series of 83 patients with coal worker's pneumoconiosis showing a good correlation of the 6MWT with lung function, but again, the correlation of this test with the radiological category of silicosis was not significant. However, our results are consistent with those of Deepak et al.,15 who in a series of 109 patients, also presented only in abstract form, noted that the distance walked gradually decreased in relation to the patient's ILO classification (a difference of 188m in patients with grade C pulmonary massive fibrosis). These differences might be explained by the inclusion in our series of a greater number of patients with complicated silicosis B and C (70 patients), all of which were classified by CT. Patients who walked less than 350m had more hospital admissions, a finding also reported in studies conducted in other respiratory diseases that showed a significant relationship between a worse outcome in the 6MWT and hospital admissions.29 Mortality in these patients was also higher, as has also been seen in other respiratory diseases in which a worse functional capacity as assessed by the 6MWT is associated with an increase in mortality.30,31
Our study has some limitations, such as the evaluation of emphysema, which was subjective, and subject selection: our decision to limit inclusion to patients with dyspnea or altered lung function tests necessarily excluded a group of subjects with silicosis from performing the test. In our experience, it is common practice to perform a single test, and while it is true that there is a tendency toward a learning effect, this has only been demonstrated in studies in patients with chronic obstructive pulmonary disease.32 To date, in all studies that evaluate the importance of the 6MWT in patients with silicosis, only 1 test has been performed.
The American Thoracic Society guidelines of 200225 do not strictly recommend the conduct of 2 tests, and the 2014 update33 specifies that the 6MWT could be performed in a single procedure, if the intention is to classify the disease or evaluate the risk of mortality or hospitalization (as is the case in our study). In the absence of properly validated reference curves for our population, we did not calculate the percentage of the predicted distance walked.3,25
In conclusion, we found abnormal 6MWT results in many patients with silicosis, especially those with complicated silicosis B and C. The presence of complicated silicosis B and C, moderate or severe emphysema, altered lung function tests (FEV1, FVC%, DLco), and desaturation during the test and during the night-time oximetry recording contribute to a poorer result in the test. Our study shows the potential usefulness of this test for assessing the functional status of patients with complicated silicosis and the important role it plays in quality of life,32 and for determining overall respiratory compromise. These results show that the 6MWT could be a very useful tool as an integral part of a prognostic scale for silicosis along with other factors such as oxygen saturation less than 90% at the end of the test, and the presence of moderate or severe emphysema, and, as such, could be used to predict which patients should be followed more closely.
AuthorshipJosé Jesús Blanco-Perez, author. Concept and design. Data interpretation. Preparation of the article. Approval of the final version.
Victoria Arnalich Montiel, co-author. Data collection. Critical review of the article. Approval of the final version.
Ángel Salgado Barreira, co-author. Data analysis and interpretation. Preparation of the article. Approval of the final version.
Maria Ángel Alvarez Moure, co-author. Data collection. Preparation of the article. Approval of the final version.
Adriana Carolina Caldera Díaz, co-author. Data collection. Critical review of the article. Approval of the final version.
Luz Cerdeira Dominguez, co-author. Conduct of 6MWT. Data collection. Critical review of the article. Approval of the final version.
Elena Gonzalez Bello, co-author. Critical review of the article. Approval of the final version.
Alberto Fernández Villar, co-author. Critical review of the article. Approval of the final version.
Francisco Javier González-Barcala, co-author. Critical review of the article. Approval of the final version.
Conflict of InterestsThe authors state that they have no conflict of interests.
We thank all the professionals Lung Function Testing Laboratory.
Please cite this article as: Blanco Pérez JJ, Arnalich Montiel V, Salgado-Barreira Á, Alvarez Moure MA, Caldera Díaz AC, Cerdeira Dominguez L, et al. La prueba de la marcha de 6 minutos como factor pronóstico y de capacidad de ejercicio en pacientes con silicosis. Arch Bronconeumol. 2019;55:88–92.