Spontaneous pneumomediastinum (PM) is an uncommon alteration defined by the presence of free air in the mediastinum that is not preceded by trauma, surgery or other medical interventions.1 Its presentation is mainly in young men, and chest pain is the most frequent symptom. Other symptoms and signs include dyspnea, cough, neck pain and subcutaneous emphysema.1–5 On occasion, chest radiograph is insufficient to detect gas in the mediastinal compartment and a CT scan is necessary.1 In the absence of an associated subjacent disease, it is considered a process with little clinical impact and its recurrence is very infrequent.1–3 Nevertheless, we have treated a patient with spontaneous NM and important gas exchange affectation who presented clinical characteristics that could cause confusion in the differential diagnosis.
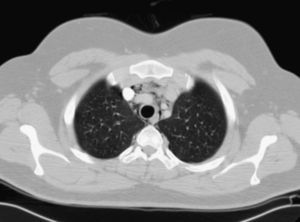
Our patient is a 24-year-old male who was admitted to the emergency department due to the sudden appearance of intense precordial pain radiating towards his back, with non-spinning vertigo and breathing difficulties due to the pain. When questioned, he only referred mild watery rhinitis during the previous four days, having received no treatment. He did not smoke, nor did he have any medical history of interest. Physical examination showed no alterations. Blood work revealed leukocytosis of 18.7×103 with 16.6×103neutrophils/μl. C-reactive protein was 20.3mg/l. Blood/arterial gas breathing room air showed pH 7.42, Pa02 54mmHg, PaCO2 35mmHg and HCO3 23mmol/l. Electrocardiogram showed a sinus rhythm with 115bpm and image of S1Q3. On chest radiograph, we observed a thin pneumopericardium line. In order to rule out pulmonary embolism, thoracic CT angiography was performed, showing no vascular defects and confirming the presence of air in the mediastinal space (Fig. 1) and pneumopericardium. The patient received analgesic treatment and oxygen. Twenty-four hours later, he was asymptomatic, with oxyhemoglobin saturation 98% (Fi02 0.21) and leukocytosis had normalized.
Spontaneous PM is considered a mild process that does not necessitate treatment.1 However, the case that we have presented showed respiratory failure, leukocytosis and clinical data that required us to rule out other processes. Although the finding of leukocytosis and neutrophilia can be frequent (in the series by Macià et al.,4 42% of the patients with spontaneous PM presented these), we have found no references to the alteration in the gas exchange in similar cases. Exceptionally, PM or tension pneumopericardium can be produced by the persistent entry of air in the mediastinal or pericardial spaces with increased pressure that can affect the venous return and the cardiac function, constituting a medical–surgical emergency1 that would explain the hypoxemia. In our patient, nevertheless, there were no data for PM or tension pneumopericardium, therefore if they had existed, there would have been transitory alterations.
Our patient had no condition associated with the development of spontaneous PM. This is not uncommon as in more than half of the patients with spontaneous PM there is no identified predisposing condition, such as asthma, interstitial disease or graft-versus-host disease.1,6 The precipitating factors that are associated with spontaneous PM are those that produce a sudden increase in intrathoracic pressure, mainly vomit, drug inhalation, intense cough and physical exercise. Nevertheless, in between 30 and 50% of patients, no precipitating factor associated with PM can be identified.1–5
We conclude that spontaneous PM, considered a process of limited clinical transcendence, can present with characteristics of greater severity than what are usually reported, although in our case there was a rapid resolution, as is usual in this process.
Please cite this article as: Kikeeva A, et al. Neumomediastino espontáneo y neumopericardio con insuficiencia respiratoria. Arch Bronconeumol. 2011;47:318-9.