Respiratory syncytial virus (RSV) infection-induced acute respiratory distress syndrome (ARDS) in previously healthy adults is rare, but the overall mortality rate is 40%-60%. Inhaled ribavirin is approved for the treatment of hospitalized infants and young children with severe lower respiratory tract infections due to RSV. We present the case of an adult female with RSV pneumonia-induced ARDS who was successfully treated with inhaled ribavirin and whose pulmonary function was restored to near normal. The role of inhaled ribavirin in adults is controversial, but it might have a therapeutic potential for severe RSV infection-induced ARDS in adults.
El síndrome de dificultad respiratoria aguda (SDRA) inducido por una infección por el virus respiratorio sincitial (VRS) en adultos previamente sanos es muy poco frecuente, pero su tasa de mortalidad global es del 40-60%. El empleo de ribavirina inhalada ha sido aprobado para el tratamiento de lactantes y niños pequeños hospitalizados por infecciones graves de vías respiratorias bajas causadas por el VRS. Presentamos el caso de una mujer adulta con un SDRA inducido por una neumonía por VRS, que fue tratada con éxito mediante el empleo de ribavirina inhalada y cuya función pulmonar se restableció hasta alcanzar casi la normalidad. El papel de la ribavirina inhalada en los adultos es objeto de controversia, pero podría tener un potencial terapéutico en los casos graves de SDRA inducida por una infección por VRS en los adultos.
Acute respiratory distress syndrome (ARDS) due to respiratory syncytial virus (RSV) is very uncommon in previously-healthy adults.1 We present the case of an adult woman with ARDS induced by RSV pneumonia who was successfully treated with inhaled ribavirin and who reached almost complete recuperation of normal lung function.
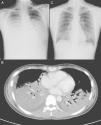
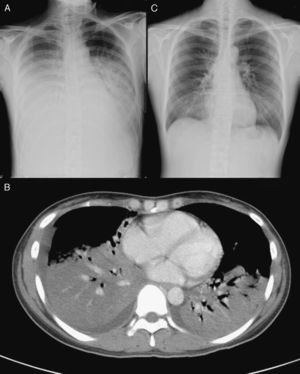
Clinical NotesA previously-healthy 32-year-old woman, a university student, was admitted to the intensive care unit (ICU) of the Taipei Veterans General Hospital, transferred from a local hospital where she had been hospitalized due to four days of high fever, cough with limited sputum production and dyspnea. The patient has never been a smoker, was following no medical treatment of any kind and her previous clinical history showed no relevant disease. Upon admittance, the initial physical examination revealed the presence of respiratory rales in both lung fields, but there was no jugular vein engorgement or any abnormal signs on heart auscultation. The laboratory analysis showed a leukocyte count of 5500/mm3, with 92% neutrophils, 0% bands, and 4% lymphocytes. Sputum Gram staining showed few polymorphonuclear neutrophils, very infrequent epithelial cells and no bacterial or fungal pathogen. Upon arriving at our hospital, the patient presented blood gas with non-rebreather oxygen mask (O2: 15 l/min) with pH=7.49, PaO2=70 mmHg, PCO2=33.5 mmHg, HCO3−=20 mmol/l and O2 saturation=95.7%. The initial chest radiograph taken in our hospital showed diffuse alveolar infiltrates in both lung fields (fig. 1A). All the symptoms and signs met ARDS criteria.
(A) Chest radiography, showing alveolar infiltrates in both lung fields. B) Chest computed tomography, showing diffuse consolidations with air bronchogram in both lower lobes, a subsegmental consolidation in the medial segment of the right middle lobe and minimal pleural effusion. C) After the treatment with inhaled ribavirin, chest radiography revealed an evident resolution of the consolidation in the lower lobes of both lungs.
We performed endotracheal intubation with mechanical ventilation support 4hours after hospitalization due to a very fast deterioration of the patient's respiratory state. After intubation, the patient required a concentration of inspired oxygen of 100%, with positive tele-expiratory pressure of 12 cm H2O, and a tidal volume of 400 ml for proper oxygenation. Thoracic CT showed the presence of diffuse consolidations with air bronchogram in both lower lobes and a subsegmental consolidation in the medial segment of the right middle lobe (fig. 1B). Fiber optic bronchoscopy revealed a small quantity of secretion of the airways in the bronchi of both sides, but there were no other alterations. Staining for bacteria, fungi and tuberculosis, as well as sputum and bronchoalveolar lavage (BAL) liquid cultures all came back negative. Enzyme-linked immunosorbent assay for IgM specific for cytomegalovirus and the simple herpes virus, antibodies and urinary antigen for legionellosis, latex test for serum cryptococcal antigen, antibody technique immunofluorescence for IgM specific for the capsid of the Epstein-Barr virus and IgM for chlamydia, particle agglutination test for the anti-body for Mycoplasma pneumoniae (M. pneumoniae) were al negative. Enzyme immunoassay (EIA) for anti-HIV in serum was also negative. Toluidine blue O stain and polymerase chain reaction testing for cytomegalovirus (CMV-PCR) in BAL liquid were negative, but EIA for the RSV antigen in BAL liquid was intensely positive. Initially, before the diagnosis of the infection by RSV, this patient had been treated with intravenous levofloxacin, imipenem, teicoplanin and methylprednisolone, but no improvement was observed in the clinical signs or symptoms or in the lung infiltrations on chest Rx 7 days after hospitalization. Thus, we administered inhaled ribavirin (Virazole; Ben Venue Laboratory, Inc; Bedford, OH) (6 g en 300 ml of normal physiological serum, continuously for 18hours/day) for three days, beginning on the eighth day after hospitalization. The follow-up chest Rx showed an evident reduction in the consolidation in both lung fields (fig. 1C) and there was a notable improvement in all the clinical signs and symptoms. Due to the severe ARDS, the patient was still not extubated. Fourteen days after hospitalization, the patient was finally and satisfactorily extubated and was later discharged 22 days after admittance with outpatient follow-up and no need for oxygen therapy. At the time of the patient's release, blood gas breathing room air was pH=7.44, PaO2=97 mmHg, PCO2=40 mmHg, HCO3−=27 mmol/l, and O2 saturation=98%. Lung function tests both before and 4 months after discharge were FVC: 79%, DLCO: 55%, DLCO/alveolar volume: 3.35 (66%) and FVC: 104%, DLCO: 72%, DLCO/alveolar volume: 3.93 (77%), respectively. There was no wheezing or dry cough after the discharge. T CD4+ cell count was initially 198/mm3 upon admittance, later recovering and reaching a value of 554/mm3 two months after discharge.
DiscussionRSV is a pathogen that is becoming more often identified in airway infections and causes important morbidity and mortality in seniors and high-risk adults, as well as in those that present subjacent cardiopulmonary disorders and/or immunosuppression.2–4 Epidemiological studies have demonstrated that RSV is only surpassed by influenza virus among the viral pathogens that cause severe diseases in seniors and in high-risk adults.5,6
ARDS due to RSV is very uncommon in previously-healthy adults. Only two cases have been reported and those patients were recuperated without using any anti-viral medication, although no data were obtained from the lung function tests.7 A study carried out in children showed that RSV infection caused a deterioration in lung function.8 In our case, the follow-up lung function tests exhibited a recuperation compared with the initial deterioration, with normal ventilatory function and a mild reduction in the gas exchange. The early treatment of ARDS due to RSV with the use of inhaled ribavirin can be useful for preserving lung function.
When the RSV enters in contact with the respiratory epithelium cells, the cytokines secreted by the epithelia infected by RSV promote the activation and recruitment of neutrophils, monocytes, memory T-cells and eosinophils in the blood towards the infected tissue. These cytokines probably contribute to producing the lesion of the airway caused by the infection by RSV.9 Various studies have highlighted that the T CD4+ cells and the T CD8+ cells participate in the defense against RSV.10 The response of cytotoxic T lymphocytes can exacerbate or also promote the clinical disease associated with the infection by RSV. In this case, the T CD4+ cell count during the infection by RSV was very low (198/mm3), but the T CD4+ cell count in the follow-up, after the recovery from the infection by RSV, was within the limits of normal. This reveals that there was a consumption of the T CD4+ cells during the infection by RSV and that the cell count recovered after the infection was cured. The dynamic change in the T CD4+ cell count could be considered one of the indicative clues of an infection by RSV. This patient may have presented an excessive response of T cytotoxic lymphocytes that led to the appearance of ARDS. So, the treatment with inhaled ribavirin can have an effect on the suppression of the viral load and can improve the recuperation from ARDS.
In our case, the diffuse consolidation in both lower lobes, as observed on Rx, did not improve despite the use of antibiotics and methylprednisolone, but did so after the use of inhaled ribavirin. The lung function tests during hospitalization showed a restrictive ventilatory deterioration and the follow-up tests found evidence of a nearly normal ventilatory function. Over the 6 months of follow-up after discharge, our patient did not show a recurrence of wheezing or respiratory difficulty, unlike another study.11 Therefore, treatment with inhaled ribavirin can reduce the respiratory consequences in adults with RSV infection.
The treatment guidelines currently in existence for RSV continue to be limited. Ribavirin is the only anti-viral agent approved for the treatment of RSV in newborns and small children hospitalized for severe RSV infection in the lower airways.12 It is possible that it may have an effect on the suppression of the viral load and improve the recuperation of ARDS, and it also may reduce the respiratory consequences in adults with RSV infection. Previous studies have demonstrated that the use of ribavirin provided a reduction in respiratory deterioration, days of hospitalization, mortality and the incidence of recurrent wheezing in infants and children with infection by RSV, as well as a preservation of the long-term lung function.13 The existing experience in immunocompetent adults is limited, therefore new studies are needed in order to evaluate the role of the treatment with inhaled ribavirin and to determine the prognosis of severe ARDS due to an infection by RSV in non-senior adults.
Conflict of interestThe authors declare having no conflict of interests.
Please cite this article as: Luo YH, et al. Tratamiento con ribavirina inhalada en el síndrome de dificultad respiratoria aguda inducida por virus respiratorio sincitial en el adulto. Arch Bronconeumol. 2011;47:315-7.