We report the case of a 24-year-old man who was treated for pulmonary tuberculosis (histological diagnosis) at the age of 16. He subsequently presented acute mumps which improved with corticosteroids. When he was 19, he was admitted for monoarthritis of the ankle and a pulmonary nodule (“chronic necrotizing granulomatous inflammation”) with negative cultures and autoimmunity testing. During admission, he developed a clinical picture consistent with granulomatous meningoencephalitis (microbiology study negative) and response to steroids.
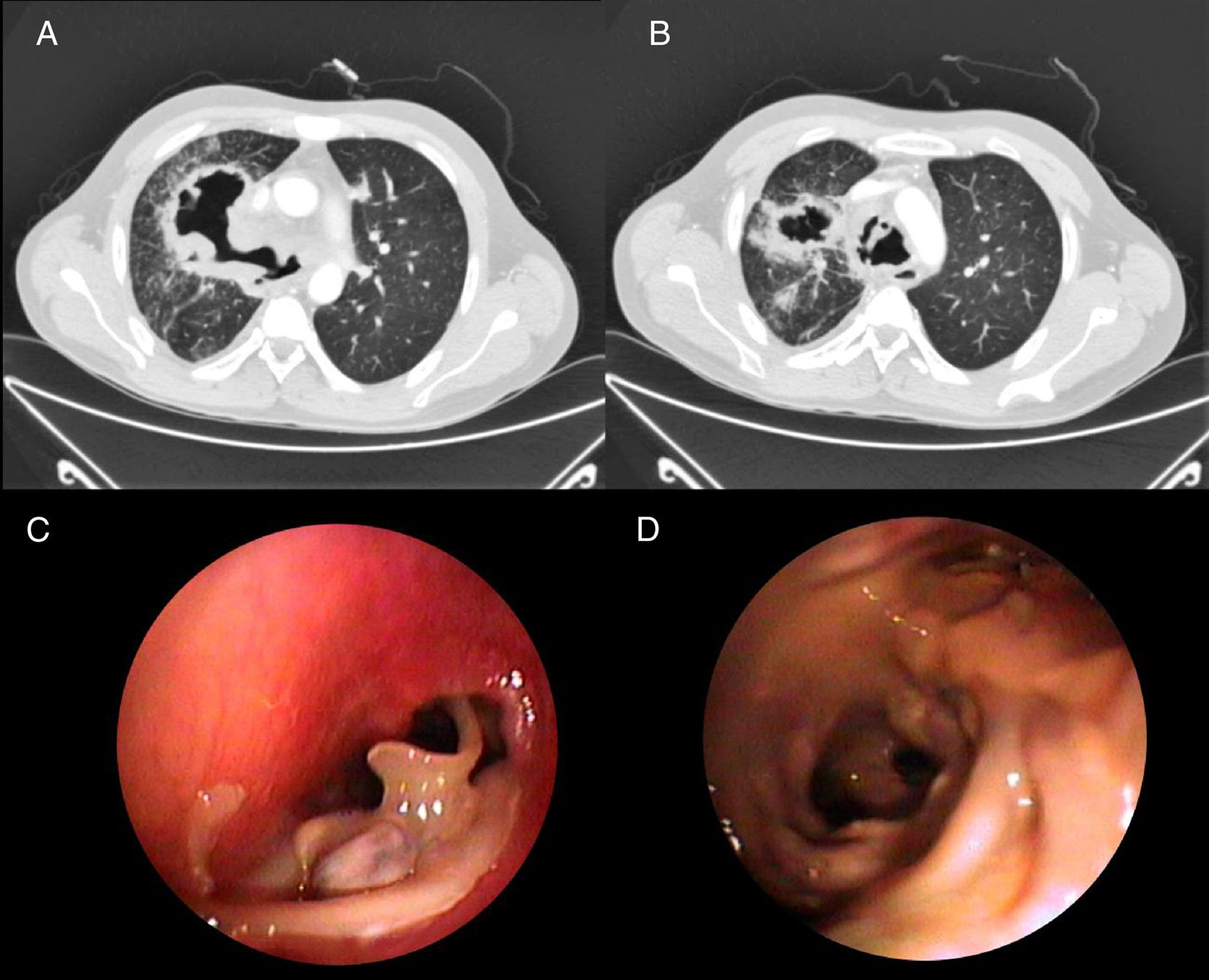
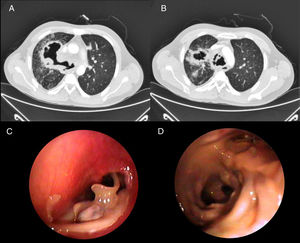
In 2017, he was admitted for fever and respiratory symptoms, with mediastinal lymphadenopathy conglomerates visualized on the chest computed tomography (CT). Successive sputum stains/cultures for mycobacteria and fungi and autoimmune markers were negative. The patient was treated with antibiotics and the corticosteroid dose was increased. Radiological images of the chest lesions showed deterioration, with thickening of the tracheal wall and necrotic masses, predominantly in the right hemithorax1,2 (Fig. 1A and B). Bronchoscopy (Fig. 1C and D) showed extensive areas of inflammation/necrosis in the main airways, with loss of wall structure and protruding fragments of cartilage. The pathology study reported granulomas, extensive necrosis, and hyaline membranes.2 Cultures for bacteria, mycobacteria, fungi, and panfungal PCR were negative.
(A and B) Chest CT showing significant concentric thickening of the tracheal wall and main bronchi, with vastly irregular tracheal and bronchial luminogram. Necrotic masses are also observed, mainly in the right hemithorax, contiguous with the bronchus of the right upper lobe. (C and D) Bronchoscopy images: (C) tracheal stenosis with friable mucosa and protrusion of fragments of cartilage; (D) division of left upper lobe and lower lobe bronchi, showing mucosa with mammilated areas.
A prosthetic trachea was ruled out due to the severity of the lesions. In view of suspected granulomatous vasculitis (Wegener's granulomatosis),1,2 steroids and cyclophosphamide were administered by intravenous bolus, but progress was unfavorable and the patient died due to massive hemoptysis.
The authors thank the Respiratory Medicine Department of the Complejo Hospitalario Ciudad de Jaén for their collaboration in the preparation of this report, especially Dr. José Nieto Serrano.
Please cite this article as: Almenara Escribano MD, Colodro Ruiz A, Martín Armada M. Inflamación granulomatosa necrosante con destrucción de la vía aérea. Arch Bronconeumol. 2018;54:389.