Stridor is a musical sound generated by the rapid, turbulent passage of air through a narrowed section of the airways.1–3 Patients with stridor should be evaluated with a complete clinical history and physical examination.2 The characteristics of stridor indicate the level of the lesion.1,2 When it occurs on inspiration, the lesion is generally supraglottic, when it is expiratory, it is located in the intrathoracic airway,1,2 and when stridor is biphasic, the stenosis is located in the trachea.2
We performed a descriptive study of children with stridor undergoing fiberoptic bronchoscopy (FB) from January 2009 to December 2013, analyzing sex, age, underlying disease, symptoms, type of stridor, fiberoptic bronchoscopy findings, treatments and FB yield. We used an Olympus® fiberoptic bronchoscopy (2.8, 3.6 and 4.8mm).
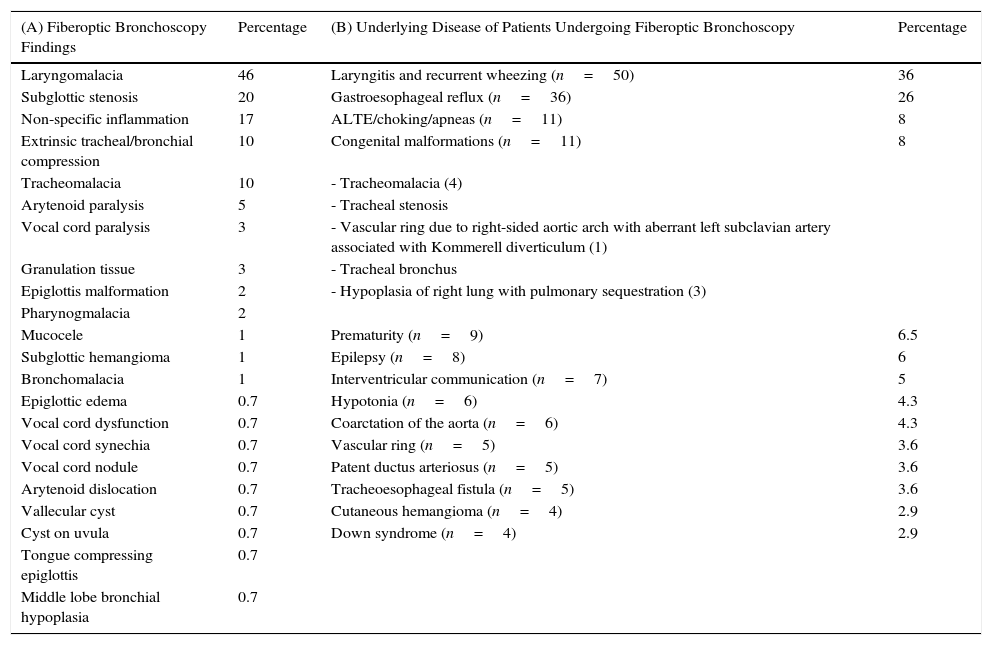
We performed 593 FBs, 138 (23%) for stridor; 63% in infants younger than 1 year, 14% in children between 1 and 2 years, 17% between 3 and 7 years and 6% in patients older than 8 years; 58% were male. The most predominant form of stridor was inspiratory (78%). Diagnostic yield was 95%, i.e., 130 patients obtained diagnostic or therapeutic benefit, while 18 of those patients required a repeat FB (12%). Most (81%) had underlying disease (Table 1). Fiberoptic bronchoscopy findings are summarized in Table 1. In 91% of cases we took a “wait and see” approach; 12 patients (9%) needed surgical treatment (6 required tracheoplasty, 2 aortopexy, 2 tracheostomy, 1 uvulectomy, and 1 laser ablation) and 2 patients with subglottic hemangioma received propanolol, with good response. A total of 8% of the patients had mild, self-limiting desaturations.
(A) Diseases Identified in the 138 Fiberoptic Bronchoscopies Performed for Stridor; in 43 Patients (31%), Multiple Findings Were Found on Fiberoptic Bronchoscopy. (B) Underlying Diseases in the 138 Patients Undergoing Fiberoptic Bronchoscopy.
| (A) Fiberoptic Bronchoscopy Findings | Percentage | (B) Underlying Disease of Patients Undergoing Fiberoptic Bronchoscopy | Percentage |
|---|---|---|---|
| Laryngomalacia | 46 | Laryngitis and recurrent wheezing (n=50) | 36 |
| Subglottic stenosis | 20 | Gastroesophageal reflux (n=36) | 26 |
| Non-specific inflammation | 17 | ALTE/choking/apneas (n=11) | 8 |
| Extrinsic tracheal/bronchial compression | 10 | Congenital malformations (n=11) | 8 |
| Tracheomalacia | 10 | - Tracheomalacia (4) | |
| Arytenoid paralysis | 5 | - Tracheal stenosis | |
| Vocal cord paralysis | 3 | - Vascular ring due to right-sided aortic arch with aberrant left subclavian artery associated with Kommerell diverticulum (1) | |
| Granulation tissue | 3 | - Tracheal bronchus | |
| Epiglottis malformation | 2 | - Hypoplasia of right lung with pulmonary sequestration (3) | |
| Pharynogmalacia | 2 | ||
| Mucocele | 1 | Prematurity (n=9) | 6.5 |
| Subglottic hemangioma | 1 | Epilepsy (n=8) | 6 |
| Bronchomalacia | 1 | Interventricular communication (n=7) | 5 |
| Epiglottic edema | 0.7 | Hypotonia (n=6) | 4.3 |
| Vocal cord dysfunction | 0.7 | Coarctation of the aorta (n=6) | 4.3 |
| Vocal cord synechia | 0.7 | Vascular ring (n=5) | 3.6 |
| Vocal cord nodule | 0.7 | Patent ductus arteriosus (n=5) | 3.6 |
| Arytenoid dislocation | 0.7 | Tracheoesophageal fistula (n=5) | 3.6 |
| Vallecular cyst | 0.7 | Cutaneous hemangioma (n=4) | 2.9 |
| Cyst on uvula | 0.7 | Down syndrome (n=4) | 2.9 |
| Tongue compressing epiglottis | 0.7 | ||
| Middle lobe bronchial hypoplasia | 0.7 |
ALTE, apparent life-threatening event.
Stridor is a symptom which requires an etiological diagnosis1–3 based on clinical history, physical examination, and direct evaluation of the airway1 with fiberoptic bronchoscopy.1–4 This is generally performed under spontaneous breathing, allowing an anatomical and functional examination of the airways.2,3 Respiratory pediatricians, ENT specialists, pediatric surgeons and/or anesthetists must work closely together to maximize the benefit of this procedure and ensure it is correctly performed. In our hospital, FB is performed in collaboration with anesthetists, who generally apply sevoflurane. In our opinion, the airway must be examined in its entirety.
Like other authors, our case series showed that laryngomalacia was the most common finding in infants with inspiratory stridor,1–3 and this condition generally resolved with a “wait and see” approach, since laryngomalacia is a result of immature laryngeal structures.2,3 The second most common disorder encountered was subglottic stenosis (15%). This percentage was high, but in our opinion there was some element of bias, as our hospital is the respiratory referral center for the south of Spain. Stridor can be caused by congenital or acquired diseases.2 The most common type is biphasic stridor associated with varying degrees of clinical airway obstruction.2 In our group of patients, all, except 1, developed symptoms after intubation. Subglottic stenoses with Cotton grades III and IV are treated by surgery, as was the case in 9% of our patients. The most common technique used was tracheoplasty with rib cartilage graft (5%).
In our opinion, FB is the technique of choice in the diagnosis of airway disorders,4,5 as it is safer and less aggressive than rigid bronchoscopy. We recommend that FB be performed in any child who presents with stridor, since this symptom is generally an indication of a banal disorder, but it can mask a life-threatening disease.1,3,5
Please cite this article as: Plácido-Paias R, Delgado-Pecellín I, González-Valencia JP. Hallazgos fibrobroncoscópicos en pacientes estudiados por estridor en un hospital de tercer nivel. Arch Bronconeumol. 2016;52:335–336.