Remarkable advances have been made in the treatment of lung cancer in recent years with the use of drugs aimed at therapeutic targets that have helped improve the prognosis of patients with disseminated disease. However, resectable lung tumors are being identified in increasing numbers of patients who cannot undergo surgery due to functional impairment, advanced age, or severe limiting comorbidities. Stereotactic body radiation therapy (SBRT) is a potentially curative alternative in the subgroup of patients with stage I lung cancers who are not candidates for surgery.1,2 SBRT uses a combination of fixed, reproducible anatomical structures as a reference for the administration of higher doses of radiation per fraction to the target lesion. For successful treatment and minimization of potential side effects, it is essential that the lesion is precisely identified. This underlying premise has supported the decision to implant fiducials within the tumor, as an essential preliminary step before delivering SBRT.
We report 2 cases of stage I lung cancer, unsuitable for surgery, in whom, after a multidisciplinary assessment by the chest tumor committee of our hospital, it was agreed to proceed with the implantation of fiducials using electromagnetic navigation (EMN) for subsequent treatment with SBRT. Our 2 patients constitute the first reported use of this technique in Spain.
The first was a 75-year-old man diagnosed with stage T1bN0M02 squamous cell lung cancer in the left upper lobe. The patient's lung function tests (showing moderate airflow obstruction, serious lung diffusion deterioration, and marked desaturation on the 6-minute walk test) and comorbidities (pulmonary hypertension group IV) were decisive factors in the choice of SBRT as optimal cancer treatment. The size of the lesion (17×19mm), its peripheral location, and a bronchus sign on radiology led us to decide on the use of EMN to guide the bronchoscopic placement of intratumoral fiducial markers.
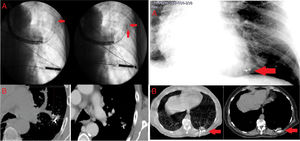
Standard flexible bronchoscopy was performed for aspiration of secretions under deep sedation with a continuous infusion of single-agent propofol. In a second procedure (after creation of the electromagnetic field), the lesion was accessed by EMN, with an estimated distance from the epicenter of 16mm. An endobronchial brush catheter (Olympus disposable cytology brush BC-202D-3010®) manually pre-loaded with a gold Visicoil® fiducial (0.35×10mm) was advanced through the extendible working channel, and the fiducial was correctly placed in the lesion under fluoroscopic control. A second Visicoil® fiducial (0.35×10mm) was placed in the same way, without complications (Fig. 1, left, A). Ten days later (waiting time required to generate airway edema and fibrosis, required for the correct anchoring of the fiducial marker3), a chest computed tomography was performed, confirming that 1 fiducial remained in place, while the other had migrated (Fig. 1, left, B).
Left (case 1). (A) Fluoroscopy view of the introduction of the endobronchial brush catheter preloaded with the fiducial via the extendible working channel (left). Placement of second intratumoral fiducial (right). (B) Chest CT after endoscopic implantation, confirming presence of the intratumoral fiducial, with migration of the second. Right (case 2). (A) Low-radiation fluoroscopy view of 2 intratumoral fiducials during bronchoscopy. (B) Chest CT after endoscopic implantation, confirming presence of 2 intratumoral fiducials with no migration.
The second case was a 60-year-old woman with a diagnosis of synchronous double lung cancer: small-cell lung cancer in the right upper lobe (lesion 1) and peripheral pulmonary nodule located in the left lower lobe, with a histological diagnosis of stage T1cN0M02 lung adenocarcinoma (lesion 2). The patient first received systemic chemotherapy with carboplatin, etoposide, and cisplatin, and as lesion 1 had shown complete tumor response, we decided to continue treatment with SBRT to lesion 2, due to its size (24×19mm), peripheral location, and a bronchus sign on radiology.
The procedure was the same as described for the first case with respect to sedation, outpatient setting, and technique; using EMN, we were able to arrive within an estimated 19mm from the epicenter of the lesion. Subsequently, 2 fiducials (Visicoil ® 0.50×10mm and Visicoil® 0.35×10mm) were placed via 2 manually preloaded endobronchial brush catheters under fluoroscopy control, without complications. Follow-up chest computed tomography carried out 10 days after the procedure confirmed the presence of both intratumoral fiducials, with no migration (Fig. 1, right).
Given the functional limitations of these patients, the chest tumor committee of our hospital decided to administer SBRT; and in view of the characteristics of the lesions (size, site, and bronchus signs), intratumoral fiducials were implanted using EMN. Several different techniques have been described for the implantation of fiducials in lung tumors, using transthoracic, intravascular, and endoscopic routes. However, the latter has a better safety profile, with fewer documented complications (lower incidence of pneumothorax, pulmonary infarctions and/or hematomas when compared with other techniques). The boom in technological advances has seen the development of several types of endoscopic approaches: standard transbronchial puncture, radial/linear endobronchial ultrasound-guided transbronchial puncture, and, more recently EMN, the latter being a safe alternative with lower complication rates than with previously described techniques.4–7
Intratumoral placement of fiducials is of great importance in SBRT, because tumor movement can be appropriately monitored during delivery of the treatment, thus reducing treatment margins and minimizing possible secondary tissue damage in adjacent healthy structures.
We thank the members of the Chest Tumor Committee of Clinical Hospital of Valladolid.
Please cite this article as: de Vega Sánchez B, Disdier Vicente C, Ponte CM, Cantalapiedra del Pie R. Colocación de fiduciales de oro intraneoplasia pulmonar mediante navegación electromagnética para tratamiento con radioterapia estereotáctica. Arch Bronconeumol. 2019;55:169–171.