We read with great interest the scientific letter by Muñiz González et al., 1 reporting the case of a 47-year-old woman who presented with cough and hemoptysis, and a cavitary lesion in the right lung. Surgical resection showed a foreign body reaction caused by silicone. She had a history of rupture of a breast prosthesis. The final diagnosis was a secondary reaction caused by migration of silicone from the ruptured prosthesis.
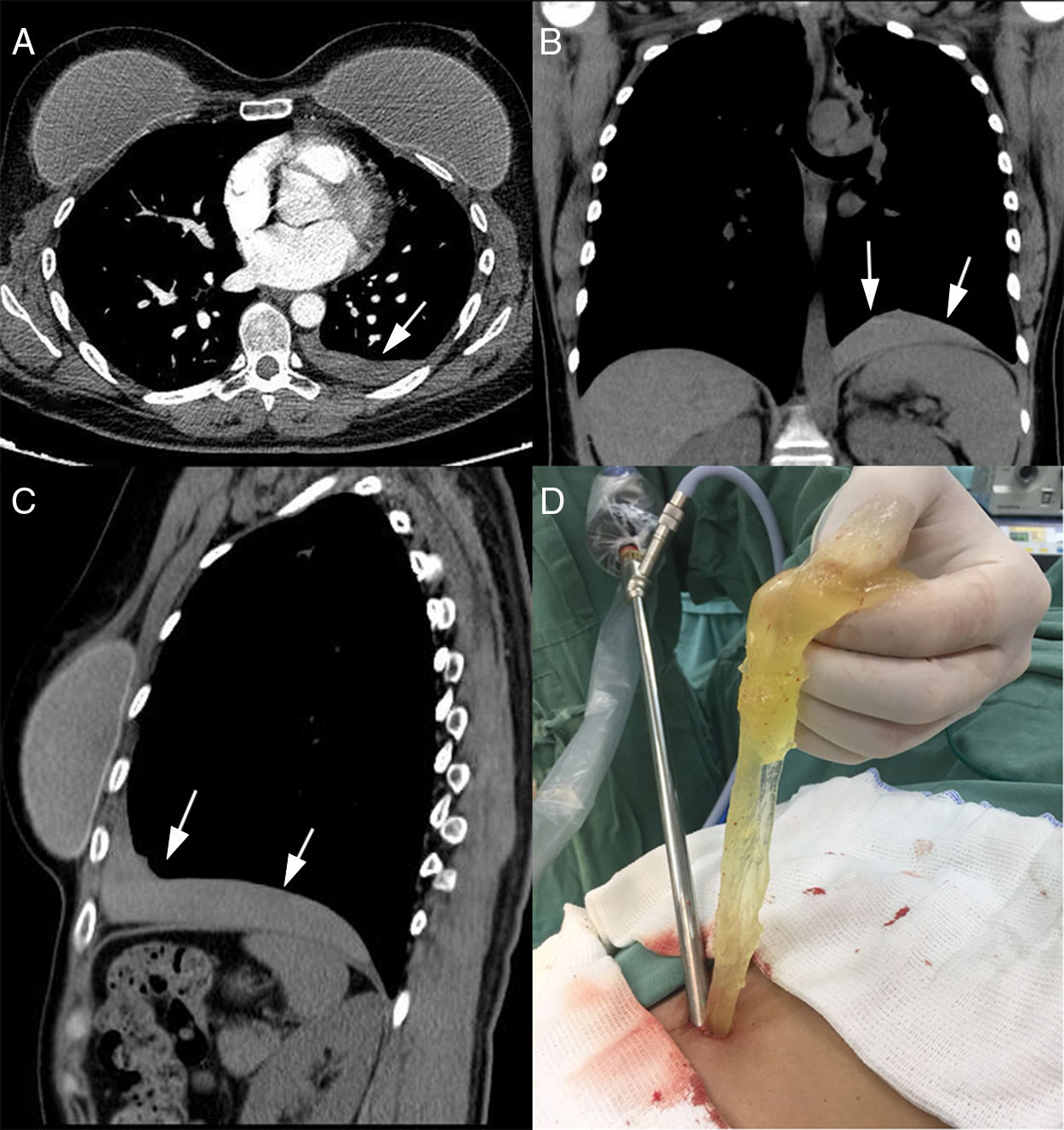
We would like to report another infrequent thoracic complication of breast prosthesis rupture: pleural silicone collection. A 51-year-old woman was admitted with abdominal pain caused by cholelithiasis. A preoperative chest X-ray showed a left pleural effusion. She was asymptomatic from a respiratory point of view. Thoracocentesis was performed, but was unsuccessful. Chest computed tomography demonstrated an elongated opacity at the base of the left hemithorax, just above the diaphragm, in the pleural cavity (Fig. 1A–C).
The patient had sustained blunt chest trauma in a motor vehicle accident 2 years previously, and had undergone drainage of the left pleural cavity. After the trauma, she noted a progressive reduction in the size of her left breast implant. Rupture was diagnosed and the prosthesis was replaced.
We therefore elected to perform a left videotoracoscopy. Exploration of the chest cavity revealed a large collection of free silicone gel in the pleural space. The silicone was evacuated manually and with suction (Fig. 1D). Clinically, the patient had an uneventful postoperative course. After 1 year, she remains asymptomatic.
Rupture of silicone breast implants is usually iatrogenic or due to trauma.2 A patient with breast implants who has sustained blunt chest injury can present a diagnostic and therapeutic challenge.
Intrathoracic migration of breast implants is a documented complication of augmentation mammoplasty.3 The prosthesis may migrate intact into the pleural cavity, usually through a defect in the chest wall caused by previous surgery.3,4 Rupture of the prosthesis also may occur without any immediate sign. Over time, the patient may notice a change in the size or shape of the breast.2
In our patient, the implant ruptured at the time of the automobile accident. Once the implant envelope had been violated, the silicone gel escaped into the local tissues, and it probably was squeezed into the pleural space at the site of entry of the pleural drain placed at the time of thoracic trauma, favored by the negative pressure of the pleural cavity.