This is a review of the different complementary techniques that are useful for optimizing home mechanical ventilation (HMV).
Airway clearance is very important in patients with HMV and many patients, particularly those with reduced peak cough flow, require airway clearance (manual or assisted) or assisted cough techniques (manual or mechanical) and suctioning procedures, in addition to ventilation.
In the case of invasive HMV, good tracheostomy cannula management is essential for success.
HMV patients may have sleep disturbances that must be taken into account. Sleep studies including complete polysomnography or respiratory polygraphy are helpful for identifying patient-ventilator asynchrony.
Other techniques, such as bronchoscopy or nutritional support, may be required in patients on HMV, particularly if percutaneous gastrostomy is required.
Information on treatment efficacy can be obtained from HMV monitoring, using methods such as pulse oximetry, capnography or the internal programs of the ventilators themselves.
Finally, the importance of the patient's subjective perception is reviewed, as this may potentially affect the success of the HMV.
La ventilación mecánica domiciliaria (VMD) precisa técnicas complementarias para optimizar el tratamiento, que son revisadas en el presente trabajo.
El manejo de las secreciones respiratorias es muy importante, ya que muchos pacientes, particularmente cuando descienden los flujos de tos, precisan la aplicación de técnicas manuales o asistidas para el manejo de secreciones, técnicas de tos asistida (manual o mecánica) y aspiración mecánica de secreciones.
Si se aplica la VMD de forma invasiva, el buen manejo de la cánula de traqueostomía es esencial para su éxito.
Las alteraciones durante el sueño pueden estar presentes en estos pacientes, siendo un aspecto a valorar, estudiadas mediante polisomnografía o poligrafía respiratoria, que además ayudan a identificar las asincronías entre el paciente y el ventilador.
Otras técnicas que pueden ser requeridas en pacientes con VMD son la fibrobroncoscopia o el soporte nutricional (especialmente si se requiere la colocación de una sonda de gastrostomía).
La monitorización de la VMD aporta información sobre la efectividad del tratamiento aplicado. Existen varios métodos para ello, como pueden ser la pulsioximetría, la capnografía o los programas internos de los ventiladores.
Finalmente, se revisa la importancia de la percepción subjetiva del paciente, ya que puede tener potencial influencia en el éxito de la VMD.
Invasive and non-invasive home mechanical ventilation (HMV) is administered in a wide range of diseases (Tables 1 and 2), with significant differences in prevalence and patterns of use.1,2 In highly dependent patients, in particular, complementary techniques are needed for HMV to be fully effective, and the aim of this article is to review those techniques.
Medical Disorders That Can Be Treated With Home Mechanical Ventilation in Adult Patients.
| Central nervous system disorders | Arnold–Chiari malformation |
| Central nervous system injuries | |
| Cerebrovascular diseases | |
| Congenital and acquired respiratory control disorders | |
| Myelomeningocele | |
| Spinal cord injuries | |
| Amyotrophic lateral sclerosis | |
| Guillain-Barré syndrome | |
| Phrenic nerve paralysis | |
| Poliomyelitis and post-polio syndrome | |
| Spinal atrophy | |
| Neuromuscular diseases | Duchenne muscular dystrophy |
| Steinert myotonic dystrophy | |
| Other muscular dystrophies | |
| Myastenia gravis | |
| Thoracic cage deformities | Thoracoplasty |
| Kyphoscoliosis | |
| Secondary musculoskeletal disorders | |
| Obesity-hypoventilation syndrome | |
| Lower airway obstructive diseases | Bronchopulmonary dysplasia |
| COPD | |
| Cystic fibrosis | |
| Other | Upper airways disorders |
| Pierre-Robin syndrome | |
| Tracheomalacia | |
| Vocal cord paralysis |
Medical Disorders That Can Be Treated With Home Mechanical Ventilation in Pediatric Patients.
| Bronchopulmonary dysplasia |
| Restrictive pulmonary parenchymal disorders |
| Thoracic cage disorders |
| Motor neuron diseases |
| Primary myopathies (e.g., Duchenne disease) |
| Spinal cord disorders |
| Congenital alveolar hypoventilation syndrome |
| Acquired alveolar hypoventilation syndrome (e.g., tumors or brain stem bleeding) |
| Myelomeningocele |
| Respiratory center development or neurological control disorders (e.g., apnea of prematurity) |
HMV patients themselves, if capable, or family members and caregivers may need to be educated and trained in airway clearance methods, including manual and instrumental techniques for assisted coughing and secretion suctioning (Table 3).
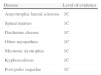
Levels of Evidence in Airway Secretion Clearance in the Diseases Most Frequently Treated With These Techniques.
| Disease | Level of evidence |
| Amyotrophic lateral sclerosis | 1C |
| Spinal injuries | 1C |
| Duchenne disease | 1C |
| Other myopathies | 1C |
| Myotonic dystrophia | 1C |
| Kyphoscoliosis | 1C |
| Post-polio sequelae | 1C |
1C: strong recommendation from low quality studies or low quality evidence (observational studies or case series).
Adapted from Make et al.24
There are several methods, such as slow expiration, autogenic drainage or forced expiration techniques aimed at improving mucociliary transport.3 These should only be applied in patients with preserved expiratory muscle function. Other manual techniques, such as percussion or clapping, manual vibration and postural drainage,4–6 have been widely studied in patients with other respiratory diseases, such as cystic fibrosis. Their utility in patients with compromised expiratory capacity has not been proven.
Instrumental Airway Clearance TechniquesOscillating and non-oscillating positive expiratory pressure (PEP) devices increase alveolar recruitment and collateral ventilation and reduce hyperinflation by increasing airflow resistance in the device outlet.3–6 Thus, positive pressure proportional to the degree of resistance of the device is generated, preventing premature closure of the airways during expiration. Moreover, they act mechanically on the rheological properties of mucus.7,8 Other systems, such as intrapulmonary percussive ventilation9,10 or external high-frequency chest-wall oscillation/compression devices, have been used in airway clearance, helping to mobilize secretions and acting on mucus viscoelasticity.11
Although these techniques have few adverse effects, gas exchange alterations and respiratory failure have been described in both healthy subjects and in subjects with chronic obstructive pulmonary disease (COPD) exacerbations.12 Similarly, expiratory muscle function must be normal.
Manual Assisted Cough TechniquesThese techniques are indicated in patients with neuromuscular diseases (NMD) and spontaneous peak cough flow (PCF) of less than 270 l/min, and in patients with other diseases involving muscle weakness and ineffective cough.13–17
These methods consist of compression of the chest and abdomen simultaneously with a cough effort. If forced vital capacity is less than 1500ml, they should be performed after achieving maximum inflation capacity, provided bulbar function is preserved. This consists of taking the maximum volume of air into the lungs in several insufflations using a manual resuscitator (Ambú®), volumetric ventilator or glossopharyngeal breathing, with the glottis closed between successive delivered volumes (breath stacking), in order to achieve high cough flows.13
When manually assisted PCFs of greater than 4L/s are achieved, there is no evidence that mechanical cough assisted techniques are more effective, and are therefore considered unnecessary. Effectiveness of this procedure is highly dependent on patient collaboration.17
Mechanically Assisted Cough TechniquesThese techniques are performed with mechanical devices that alternately generate positive pressure (insufflation) followed by negative pressure (exsufflation), causing airflows that can transport secretions from distal to proximal regions. They can be administered via a leak-free oronasal interface, or via a tracheostomy or orotracheal tube. At present, 2 devices for mechanical insufflation/exsufflation are available: Respironics Cough-Assist® and the newer Respironics Cough-Assist E70® that is more portable, can determine PCF and volumes, and offers a combination of oscillation and pressure cycling,18 in addition to other devices that may be on the market. High frequency oscillation in association with mechanically assisted cough does not affect PCF or volumes in clinically stable amyotrophic lateral sclerosis (ALS) patients.19 These techniques must be applied at least 3 times a day, and on demand if they lead to an increase in secretions or associated desaturations.13–17
Mechanical assisted cough is indicated in patients with NMD and PCF less than 270 l/min, and in patients with other diseases involving muscle weakness and ineffective cough, provided bulbar function is at least partially preserved.13–17 If bulbar muscles are severely compromised, Cough-Assist is ineffective for non-invasive airway secretion clearance, since upper airway collapse or glottal closure during the exsufflation phase with the subsequent retention of respiratory secretions below the level of the collapse has been described in these patients.20
As a rule, 6–8 cycles of mechanical insufflation–exsufflation should be applied, although this must be tailored to each patient, depending on tolerability, efficacy and experience with the device. The technique can be repeated in acute situations until secretions are resolved or desaturation is reversed. The device can be used in either automatic or manual mode, facilitating coordination between the patient and the caregiver/nurse. When used with an oronasal interface, initial pressures of +20 to −20cmH2O are programmed and gradually increased, depending on tolerance, to more effective levels of +40 to −40 cmH2O. An artificial lung model was used to demonstrate that with normal impedance at insufflation pressures of +40cmH2O, exsufflation pressures of −40cmH2O, 2-second insufflation times, 3-s exsufflation times and 1-s pauses, exsufflation flows >270L/min were achieved.13–17,21 When the impedance of the artificial lung was modified, exsufflation flows obtained in these parameters varied according to changes in resistance and compliance.16
It has been reported that in stable adults, pressures lower than ±30cmH2O are ineffective, and in acute situations, where airway resistance is increased due to secretion retention or reduction of thoracopulmonary compliance, higher pressures may be necessary.20,21
Secretion SuctioningSecretions can be best managed with a combination of mechanical insufflation–exsufflation devices and with catheter suctioning, particularly in NMD patients. Secretions are cleared via a catheter connected to a suction device. Caregivers must be trained in the use of this technique and in the prevention of complications, such as obstruction by mucus plugs. The diameter of the suction tube must exceed than half the internal diameter of the cannula or more than 70% in children. A negative pressure of 120–140mmHg is recommended in adults, 80–120mmHg in adolescents, 80–100mmHg in children and 60–80mmHg in neonates. Insertion should be shallow to avoid adverse effects, and should not last longer than 15s, since vigorous suctioning may cause endobronchial lesions. One of the most significant drawbacks is that due to the anatomy of the bronchi, the right bronchial tree is accessed in 90% of cases, leading to incomplete suctioning.16,22 When suctioning higher regions, the procedure should be combined with Cough Assist, ensuring that the suction tube does not pass beyond the distal end of the cannula. This technique is more complete and less traumatic, and areas that are inaccessible to conventional aspiration can be cleared.23
Invasive Airway Access: TracheostomyWhen non-invasive ventilation (NIV) is ineffective due to unsuccessful non-invasive assisted cough or severe bulbar involvement, a tracheostomy should be proposed to the patient. The standard indication is a predicted FVC<50%, although this threshold varies depending on the report.24 If the patient has an acute disease, weaning and decannulation may be started after recovery if progress permits.25 However, if the patient has NMD with severe bulbar involvement, non-invasive support will fail and the tracheostomy must be maintained.26,27 The choice of HMV, whether invasive or non-invasive, must be discussed at an early stage to accommodate the wishes of the patient and family members. This is a decision that should never be taken during an acute decompensation without knowledge of the patient's wishes in this respect,28 and therefore a prior respiratory evaluation must be performed to detect early signs of respiratory failure and discuss the options with the patient and all those involved, both family and professionals. In these situations an advance directive or living will, already granted legal standing several autonomous communities in Spain since 2002, is an invaluable document and something we would always recommend. It allows patients to express, before they are no longer in a situation to do so personally, how they would, at least, not like to die, thus saving the family the distress of authorizing or refusing a particular treatment.26
Tracheostomy TubesCuffed tracheostomy tubes probably cause fewer long-term problems and are the most suitable choice when non-invasive methods have failed. A fenestrated tube will allow the patient to talk when the cannula outlet is covered (bulbar involvement permitting). In order to prevent ulcers or granulomas, the position of the tube must be checked by fiberoptic bronchoscopy (FB) during placement to ensure neither the fenestration nor the distal end come in contact with the tracheal mucous membrane. When patients are unable to manipulate the tube themselves, a reliable alert system is essential, along with a person always available to help.28
For safety reasons, tubes must always have an internal cannula that can be immediately extracted in case of obstruction.26 Cuffless tubes generally allow good alveolar ventilation and airway clearance until bulbar involvement reaches the critical point at which leaks become excessive or saliva suctioning is uncomfortable or causes hypoxemia. Cuffless tubes may help phonation in patients on 24-h invasive ventilation, provided bulbar function is maintained. In patients on invasive ventilation <24h, the use of fenestrated tubes may be useful for permitting phonation during break times. When cuffed tubes are used, filling pressure must be less than 25mmHg, and in patients without gastrostomy, the cuff should not be inflated at mealtimes, since this may increase mechanical interference with swallowing and lead to aspiration.
In the case of part-time invasive ventilation, provided the fenestration is seen on FB to be well-located, fenestrated tubes reduce the ventilatory effort and allow the patient to talk during break times.28
Airway Clearance via TracheostomyIn these cases, airway secretion clearance methods are similar to those described above, with some small adjustments.26 It is important to check that caregivers are performing suctioning correctly and the home care materials (tubes, spare parts, suction device, etc.) are appropriate. For tracheal suctioning, the catheter should be inserted to a shallow depth and deep suctioning should be avoided to prevent injury to the tracheobronchial mucosa. Moreover, as described above, deeper penetration generally only gives access to the right bronchial tree. To reduce the risk of complications associated with tracheal suctioning, it has been suggested that mechanical cough assistance should be applied first (see section in this review). Suctioning devices must be clean, but a sterile environment is not necessary. No specific studies have been designed to determine the correct time for performing suctioning. Experts suggest following the patient's feeling, increased ventilator peak pressures and SpO2 decompensations. Routine instillation of serum via the catheter should be avoided. Guidelines recommend heat and moisture-retaining filters, rather than the use of heat and moisture exchangers during ventilation via tracheostomy.29,30
Main Complications of Tracheostomy Mechanical VentilationTracheal lesions can be avoided with good practices but respiratory infections remain the most common complications in these patients. Protocols that facilitate early therapeutic responses must be used, and effective alert systems for avoiding severe or fatal episodes must be available.31
Care of the Tracheostomy Tube at Home. Tube ChangesThere is little information in the literature regarding how often a tube should be changed: in general, the recommendations have been derived from expert opinion.
The tube should be first changed by expert, trained personnel between 7 and 14 days after placement. Successive changes will depend on the manufacturer's recommendations, the condition of the patient, and clinical requirements. Most tubes consist of an exterior tube and 2 internal cannulae to assist in daily cleaning and extend duration of use. In general, the whole tube should be changed every 30–90 days.32
Sleep and Home Mechanical VentilationHMV is associated with sleep changes, either due to the underlying disease or the ventilation process (leaks or asynchrony). Sleep studies are useful for diagnosing or monitoring response to treatment, particularly patient-ventilator synchrony (the primary factor in HMV tolerance and efficacy), with a view to adjusting ventilator parameters.33,34
Sleep and Home Mechanical Ventilation in Neuromuscular DiseasesPatients with NMD have fragmented sleep, low sleep efficiency, increased phase 1, reduced REM sleep, central and mixed apnea, hypoventilation and, less frequently, obstructive sleep apneas.35,36 HMV can improve respiratory parameters, survival and quality of life.37–40 Improved oxygenation has also been described.41
There is no consensus on the need for a sleep study, whether polysomnography (PSG) or respiratory polygraphy (RP), at the start and during the course of HMV. Studies have found evidence for42,43 and against44,45 PSG or RP.
Current evidence suggests that nocturnal oximetry, ideally with capnography, and in case of doubt, PSG, should be performed in non-HMV patients with NMD with suspected sleep alterations. A PSG is not required before starting HMV, but once the respiratory therapy has been introduced, PSG sleep study can be performed in case of poor tolerance, failure to correct symptoms and/or blood gas parameters.44,46
Sleep and Home Mechanical Ventilation in Chronic Obstructive Pulmonary DiseasePatients with COPD have fragmented sleep and frequent desaturations during REM sleep.47–49 Daytime O2 saturation at rest is one of the best predictors of nocturnal desaturation,50,51 although other factors, such as obesity, hypercapnia or sleep apnea-hypopnea syndrome (SAHS) must be taken into account.52
A recent meta-analysis has shown that HMV in stable hypercapnic COPD patients has no clinical or statistical effect on gas exchange, exercise tolerance, quality of life, lung function or sleep efficiency.53
Results regarding the impact of NIV on sleep efficiency are contradictory.54–57 PSG or RP is performed if there is a suspicion of associated SAHS and in patients with dyspnea and breathing difficulties despite ventilation, with a view to adjusting ventilator parameters.58
Sleep and Home Mechanical Ventilation in KyphoscoliosisAlthough determination of lung function and nocturnal oximetry is a useful tool alongside daytime capnography for documenting hypoventilation requiring the start of HMV, PSG is a more sensitive test for determining nocturnal hypoventilation and the possible coexistence of SAHS.59
HMV is offered in the case of hypercapnic chronic respiratory failure; patients without hypercapnia can be managed cautiously with supplementary oxygen therapy.60–62
Data are available neither on ventilatory mode and HMV parameters, beyond their use in resolving nocturnal hypoventilation, hypoxia and SAHS, nor on the site of initiation of therapy, supervision, support and monitoring.63
Sleep and Home Mechanical Ventilation in Obesity-Hypoventilation SyndromeSleep disorders are very common in patients with obesity-hypoventilation syndrome (OHS), although they not included in the definition of this syndrome. Moreover about 80%–90% of SAHS patients also have sleep disorders.64,65 Hypoventilation without SAHS and central apneas are more uncommon.66
Most patients can be managed with bilevel NIV, and CPAP can be effective in cases with mild OHS and SAHS. PSG, nocturnal oximetry and blood gases are used to determine response to treatment. PSG is useful for titration and for confirming the efficacy of ventilator parameters.67
Fiberoptic Bronchoscopy and Home Mechanical VentilationFB is a diagnostic and therapeutic technique that may be indicated in situations of acute respiratory failure or in HMV-dependent patients. The use of ventilation during FB may help prevent complications and improve ventilation during the test.68 Several studies have shown that NIV can be applied safely with the use of various interfaces (helmet, face, oronasal or nasal mask).69–71 Thus, the need for ventilation is not necessarily an obstacle to conducting this technique if needed, provided it is performed by expert staff in an appropriate setting.72
Nutrition and Home Mechanical VentilationNutrition is a basic aspect of care of HMV patients, and is a prognostic factor. Nutritional advice or provision of supplements may be sufficient, but sometimes a gastrostomy tube needs to be inserted, particularly in patients with NMV.27,73 This can be safely placed in ventilated patients, even in those with advanced deterioration.74
Home Mechanical Ventilation MonitoringMonitoring is performed for two reasons: to observe the situation (safety) and to provide information (for adjustment or correction of parameters). There are various methods for the non-invasive monitoring of the effects of HMV (Table 4).
Methods for Home Mechanical Ventilation Monitoring.
| Method | Significance | Advantages | Limitations |
| Pulse oximetry | Desaturations are considered factors for certain neurocognitive and cardiovascular disorders | Low cost, simple to use, rapid preparation and results | Movement artifacts, influence of tissue perfusion, low specificity |
| Capnography | Alveolar ventilation marker | Simple to use, rapid preparation and results | Occasional lack of concordance with PaCO2, cost |
| Inbuilt ventilator systems | Information about respiratory mechanics (tidal volume, minute volume, distensibility, respiratory events, leakages, etc.) | Multiple signals available, real time information, record of history | Variability between devices, limited validation |
| Sleep testing | Complete information during sleep | Multiple channels available | Limited access |
Oxygenation is essential in HMV. Nocturnal desaturation is thought to be one of the primary factors in neurocognitive disorders and the cardiovascular consequences of chronic respiratory failure. Although no guidelines have been established, SpO2 (particularly nocturnal recording) is one of the most widely recommended instruments.75,76
There are several disadvantages, including measurement artifacts (movements) and the effect of peripheral tissue perfusion. Moreover, there is wide device-related variability, depending on sampling frequency (range 2–21s). The precision of SpO2 in sleep studies has been reported to be 2%–6% compared to blood gas determinations.77,78 The greatest problem is its low specificity, since the consequences (desaturations) are measured, but the multiple causes (upper airway instability, apneas, reduced ventilatory drive, asynchrony or air leaks) are not recorded.79
The main advantages of the method include low cost, simplicity, rapid preparation and quick results (a few seconds, in both cases).
CapnographyCO2 measurement determines the adequacy of alveolar ventilation. There are 2 techniques:
- (a)
Determination of end-tidal CO2 (PETCO2). It is not widely used due to several limitations. The PETCO2–PaCO2 gradient depends on the VD/VT ratio. Reliability is reduced when it is used at night (physiological dip during sleep) or in patients with VD/VT ratio changes. Moreover, leaks in the HMV interface cause technical problems.80
- (b)
Transcutaneous CO2 (PtcCO2) determination. This measurement is based on the finding that CO2 solubility is high in the tissues, and it therefore diffuses rapidly through the skin, where an electrode is used to measure PtcCO2. There is good concordance between this method and invasive blood gas measurement, even during mechanical ventilation.81
The major limitations are local discomfort associated with incorrect use (mainly skin burns), the importance of correct electrode positioning, the use of disposable materials (membranes, gas, etc.), the need for regular calibration and the cost of the equipment.81
New devices that overcome former problems such as regular calibration or local discomfort have recently been developed, and the use of these systems should be considered as a non-invasive alternative to blood gas determination.33,82
Ventilators With Inbuilt Analytical SystemsVentilators are usually equipped with respiratory polygraphy systems (developed by the manufacturers) that provide data on respiratory mechanics in the ventilated patient. This information is derived from direct measurements (sensors) or estimates (mathematical algorithms).83,84
The reliability of estimated tidal volume and leakage varies widely.85 Moreover, few studies have examined the impact of these parameters in standard clinical practice.86,87 In view of the limited data and the lack of recommendations from scientific societies, these systems have been attributed a low level of evidence.33
In view of the reliability of the results obtained, it seems clear that these algorithms should either be standardized or independent monitoring systems should be developed.88
Patient's Subjective PerceptionFew studies have been conducted on the patients’ point of view and their satisfaction with HMV,89 although this is an important aspect of the quality of services.90–92 Home ventilators vary widely in terms of technical features93 and are not easy to use, being neither manageable nor user-friendly for either the physician94 or the patient.95
NMD patients receiving HMV take a different view from prescribing physicians: the latter are more inclined to prescribe new technologies, while patients are more reluctant to try them, due to a lack of information.96
Finally, interface choice is also a key aspect in the success of HMV,97 and the final selection must reflect a combination of patient preference and efficacy, although patient preference in HMV has not been studied in randomized trials.98,99
Future OutlookThere appears to be a need for studies validating inbuilt ventilator monitoring systems that provide reliable data to assist in decision-making. These monitoring systems should, ideally, provide remote access, with the corresponding potential benefits for the patient and for the healthcare system (resource utilization).100 Furthermore, access in real time and immediate availability of full monitoring records could provide the most complete information possible for decision-making. Perhaps the most recent advances in the field of telemedicine could be used to achieve these ends.87,101
FundingThis paper received no funding of any type.
Conflicts of InterestThe authors state that they have no conflicts of interest.
Please cite this article as: Chiner E, Sancho-Chust JN, Landete P, Senent C, Gómez-Merino E. Técnicas complementarias a la ventilación mecánica domiciliaria. Año SEPAR 2014. Arch Bronconeumol. 2014;50:546–535.