Bronchial schwannomas, also known as granular cell tumors and myoblastomas, are uncommon benign tumors1 that rarely occur in the bronchi. Disease course is benign and treatment of choice is surgery.
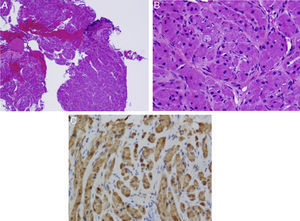
A 40-year-old woman, smoker of 20 pack-years, with clinical criteria for chronic bronchitis, presented in the emergency department with a 2-day history of fever 39°C, general malaise, dry cough, myalgia, headache, and pharyngeal pain. Chest X-ray revealed alveolar infiltrate in the left upper lobe (LUL). A diagnosis of community-acquired pneumonia was given, and she was prescribed levofloxacin 500mg for 7 days in an outpatient setting. Four weeks later, a radiological control was performed and the patient was referred to the respiratory medicine department. During anamnesis, she reported a long history of episodes of lower respiratory tract infections. Physical examination and blood test results were normal. Chest X-ray showed LUL atelectasis with left hilar elevation. Chest computed tomography revealed a 2cm nodular lesion in the LUL, causing partial atelectasis, with no mediastinal or hilar lymphadenopathies. Spirometric results were normal. Fiberoptic bronchoscopy showed a pedunculated lesion in the left bronchial tree, obstructing the upper lobe. The lesion surface was smooth, shiny and vascularized. It was contingent on the carina dividing the lobes, and there was no adhesion to the lateral walls. Biopsy showed fusiform, polygonal cells and granular cytoplasm with immunohistochemical (IHC) expression of neuron-specific enolase, S100 protein and vimentin (Fig. 1), indicative of LUL schwannoma.
(A) An area of bronchial epithelium can be seen on lower magnification (top right, darker area). The rest of the sample consists of tumor tissue. (B) Fusiform cells and granular cytoplasma can been seen on greater magnification. Bronchial schwannoma or granular cell tumor. (C) Immunohistochemistry positive for S100 (darker staining).
The LUL was lobectomized, and the patient did not require any further treatment.
Schwannomas are extremely rare1 benign tumors, originating in the Schwann cells that produce the myelin sheath of the peripheral nerves. The first case was described by Feckner in 1938, and at least 80 cases have been published since then. These are slow-growing tumors, that do not infiltrate the neuronal axon, but which can affect nerve conduction by extrinsic compression. They appear in wide range of sites, the most common of which are the skin and the tongue.2 Endobronchial presentation occurs in only 6% of cases.2,3
Schwannomas generally occur in middle age, and no differences are observed between sexes.1 Clinical presentation can very, and is determined by the size and location. Early symptoms include asthma, unproductive cough, recurrent infections (as in our case), fever, dyspnea and hemoptysis.2,3 Lesions tend to develop in the large bronchi or in bifurcatons.3,4 Up to 25% may be multiple, and they can even mimic metastasis, if they occur concomitantly with other neoplasms.2 Radiographs can be useful in differential diagnosis, but definitive diagnosis is usually obtained on fiberoptic bronchoscopy for atelectasis and secondary pneumonia, as in our case.2,3
On histological examination, tumor cells are polygonal and fusiform, with granular cytoplasma. On IHC, antigen expression is positive for S100 protein, vimentin, neuron-specific enolase, and negative for keratins.4
While endoscopic resection has been recommended for treating small lesions, surgical resection is still the treatment of choice due to the risk of recurrence, irrespective of tumor size.3,5 Prognosis is favorable, and mean survival after surgery is longer than 5 years.1
Conflict of InterestsThe authors state that they have no conflict of interests.
Please cite this article as: Landete P, Chiner E, Sancho-Chust JN, Pérez-Ferrer P. Schwannoma bronquial, un tumor poco frecuente. Arch Bronconeumol. 2015;51:471–472.