Lung transplantation has become a standard treatment for patients with terminal respiratory failure who have exhausted all therapeutic alternatives and have a limited life expectancy.
Lobar transplantation, as a variant of lung trasnplantation, involves the use of lung lobes instead of the entire graft. The objective is to adapt the size of the donor organ to the chest cavity of the recipient. This way, patients with severe pleural cavity restriction, either due to their underlying disease or because they are pediatric patients, avoid excesive time on the waiting list until a suitable sized donor is found. Several groups have published their experience with lobar transplantation and have reported acceptable results.1,2
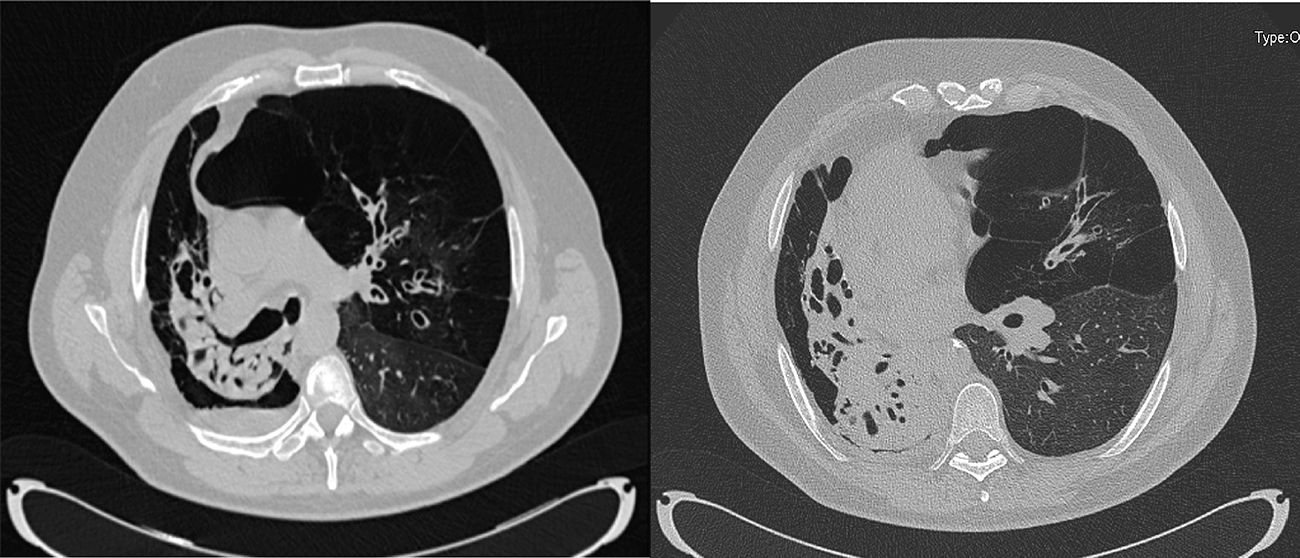
We report the case of a 54-year-old man with COPD diagnosis associated with right pulmonary parenchymal destruction, especially of the right lower lobe, due to bronchiectasis (Fig. 1). In fact, lung perfusion scintigraphy determined 6.5% perfusion on the right side and 93.5% on the left. Such a significant restriction of the right cavity led us to consider a right-sided bilobar transplant (middle and right lower lobes) via posterolateral thoracotomy, followed by a left-sided single-lung transplant using central extracorporeal membrane oxygenation (ECMO), in the supine position. The unusual right-sided approach and the manner of protecting the newly implanted lobar graft are 2 technical details that make this case interesting.
CT slices showing a collapsed right lung due to the presence of multiple bronchiectasis. Only the areas of emphysematous lung are aerated, with bullous changes. A small air-fluid level suggestive of superinfection over the bullous parenchyma can also be visualized. Moreover, major hyperinflation is present in the left lung with extensive areas of panacinar emphysema in the upper lobe. This hyperinflation, along with the collapse of the right lung, produces a significant shift in the mediastinum toward the contralateral side.
With regard to lung volumes, the recipient had a total lung capacity of 6.8l predicted and 6.5l real. The donor was 60 years old, and had a PaO2/FiO2 ratio of 436, a normal chest X-ray and bronchoscopy, and a total lung capacity of 6.7l.
The recipient was initially positioned in left lateral decubitus, and a right posterolateral thoracotomy was performed. After removing lung adhesionsespecially in the right lower lobe destroyed by bronchiectasis, a right pneumonectomy was carried out. The pulmonary hilum was prepared in a conventional manner, opening the pericardium around the pulmonary veins and artery and cutting the bronchus 2 cartilages away from the main carina. Meanwhile, a right upper lobectomy was performed on the back tablet, preserving the middle and lower lobes. In order to retain a sufficiently large left atrial cuff, the right superior pulmonary vein was ligated outside instead of cutting the atrium.
Despite the unusual approach and the longer procedure time, the right transplantation was completed without incident. The pulmonary artery was then isolated with a double tourniquet, keeping it closed in order to protect the newly transplanted lobar graft from anterograde blood flow. In that situation, without arterial flow toward the graft and without ventilation, the posterolateral thoracotomy was closed and the patient was placed in a supine position. A bilateral thoracotomy with a transverse sternotomy was performed and central ECMO was initiated. The tourniquet on the right pulmonary artery was then opened, allowing reperfusion of the lobar graft after starting the ventilation. Left lung transplantation was then performed in the usual manner. Cold ischemia time was 8 and 10h for the right and left grafts, respectively.
Given the recipient's good heart function, confirmed during the procedure with transesophageal echocardiography, and in order to protect the grafts, we decided to switch central ECMO to a peripheral veno-venous configuration. We did this using the femoral vein for the extraction of blood and the internal jugular vein to infuse the blood oxygenated by assistance.
The first chest x-ray showed bilateral edema, and given that the patient was on venous-venous ECMO, the case was classified as primary graft dysfunction grade 33. However, 6 days after transplantation, PaO2/FiO2 ratio improved remarkably and the chest X-ray was almost normal Therefore ECMO therapy was discontinued. An early tracheostomy was performed on postoperative day 4, and the patient was weaned off all ventilatory support by day 50. ICU and hospital lenght of stay were 54 and 122 days respectively. Other complications included superficial dehiscence of the surgical incision, which was treated with vacuum therapy. The patient also developed an episode of acute cellular rejection A1 and renal failure, but both situations had been resolved by the time of discharge.
In short, lobar transplantation is a valuable option to optimize lung donation and to adapt the graft size in special situations, such as pediatric cases or small chest cavities. Usually these recipients cannot wait for a perfect sized donor. However, it is important to consider some type of cardiorespiratory assistance to protect lobar grafts during both the intraoperative (cardiopulmonary bypass or ECMO) and postoperative period (mainly ECMO), depending on the clinical scenario and preferences of the surgical group. In this particular case, lobar transplantation was combined with an unusual approach, a posterolateral thoracotomy. For that reason, until central ECMO was established, we decided to maintain the lobar graft without blood flow and without ventilation.
Other alternative surgical strategies for this transplant were considered, but ruled out. The possibility of right pneumonectomy, with the implantation of a single left lung, was rejected due to problems that might occur in association with the healing of the bronchial stump and pneumonectomy cavity. Performing the transplant using peripheral veno-arterial ECMO was also ruled out due to the risk of cannulas displacement during intraoperative positional changes.
In conclusion, given that the patient's right cavity could only accommodate 2 lobes, and that the best approach for this procedure was posterolateral thoracotomy, we believe that maintaining the bilobar graft without blood flow or ventilation until the establishment of cardiorespiratory assistance was a valid strategy.
We thank the Departments of Respiratory Medicine, Anesthesiology and Transplant Coordination of the Hospital Universitario Puerta de Hierro-Majadahonda.
Please cite this article as: Campo-Cañaveral de la Cruz JL, Gómez de Antonio D, Sánchez Calle Á, Romero Román A. Trasplante pulmonar bilateral en un paciente con una restricción severa de la cavidad pleural derecha. Arch Bronconeumol. 2019;55:271–272.