We report the case of a 19-year-old man with a history of post-traumatic subdural hematoma in December 2014.
He attended the emergency department of our hospital with a clinical picture suggestive of acute respiratory infection and radiological image consistent with right basal pneumonia. He denied any previous episodes of repeated catarrh or bloody expectoration.
A chest radiograph performed during admission revealed a well-defined, homogeneous mass in the lower third of the right hemithorax, obliterating the hemidiaphragm, with no clear picture of air bronchogram in the interior. Given the homogeneous aspect of the mass, a chest CT was requested, also during admission, which described an area of lung consolidation 9cm in diameter with peripheral bronchogram in the posterior and medial segment of the right lower lobe. Empirical antibiotic treatment began, and after good clinical progress and partial resolution of the radiological findings, the patient was discharged with a diagnosis of community-acquired pneumonia.
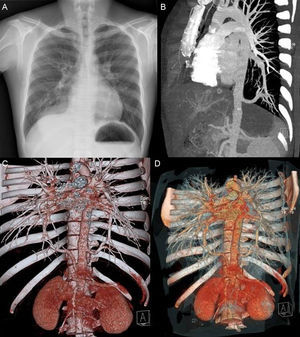
In a follow-up visit, partial persistence of the right homogeneous mass was noted, and a “tubular opacity” was observed in the left base behind the cardiac silhouette (Fig. 1A), leading us to a diagnosis of pulmonary sequestration. An angiotomography was requested, which revealed pulmonary sequestration (PS) in the right lower lung base, with no fissure separating it from the rest of the pulmonary parenchyma, irrigated by an artery originating in the abdominal aorta, and venous drainage to the left atrium via the right inferior pulmonary vein; PS in the left posterior lung base, partial fissure separating it from the rest of the pulmonary parenchyma, irrigated by an artery originating in the thoracic artery, and venous drainage to the left atrium via the left lower pulmonary vein (Fig. 1B–D).
(A) PA chest radiograph showing a well-defined mass in the right lower lobe, containing no apparent air bronchogram, and left retrocardiac tubular opacity corresponding to a feeder vein originating from a branch of the abdominal aorta. (B–D) Reconstruction of chest CT showing vessels feeding both sequestrations. In the right side, the artery originating in the abdominal aorta can be seen with its venous drainage to the left atrium, via the right inferior pulmonary vein. In the left side, the artery originating in the thoracic aorta can be seen with its venous drainage to the left atrium, via the left inferior pulmonary vein.
In view of the CT findings, the patient was referred to the reference thoracic surgery unit for surgical evaluation with a diagnosis of bilateral PS. Atypical ablation of the right lower lobe was performed by right video-assisted minithoracotomy with ligation of the artery originating in the abdominal aorta. In a second stage, 2 months later, atypical ablation of the left lower lobe was performed by left video-assisted minithoracotomy, with release of the sequestered artery and the inferior pulmonary vein. Intraoperative diagnoses were: right and left intralobar PS with accessory fissure in the left lower lobe, irrigated by a direct branch from the aorta. The pathology report described pulmonary parenchyma lined with visceral pleura, with isolated foci of pulmonary fibrosis and dilated bronchi, findings consistent with intralobar PS in the left lower lobe and right lower lobe.
PS is a rare malformation, and diagnosis is generally made early in life. The treatment of choice is segmentectomy by thoracotomy. Most intralobar PS are unilateral, and bilateral PS are very rare. The general incidence of PS ranges between 0.15% and 1.8%; the exact statistics of bilateral PS have not yet been determined, but it is known to be extremely rare.1
The radiological image of intralobar sequestration can vary: it can be a well-defined homogeneous mass, an air- or fluid-filled cystic lesion, a hyperlucent and hypovascular region, or a combination of all of these.2 Presentation may also be unusual, as in our case, manifesting with only a subtle area of tubular opacity in the lower lobe that might represent the systemic vessels or venous drainage associated with the lesion.3
Several case reviews published over the years have reported very few bilateral sequestrations, an example being the review published by Wei Y and Li F in 2011, in which only 3 of 2625 reviewed cases were bilateral; 2 patients both with intralobar PS, as in our case.4
With respect to treatment, surgical resection of the smallest amount of pulmonary parenchyma possible has been compared with angiographic embolization in newborns: the safest and most effective method appears to be surgical resection,5 although there have been reports of asymptomatic patients successfully treated with embolization.2
Although many presentations of PS have been described in the literature, we must remember that slow-to-resolve pneumonias may conceal this entity, a fact that, along with the tubular opacity, guided us toward the diagnosis. Moreover, it is unclear how many cases of bilateral PS exist in Spain, and we believe that it would be of interest to make a larger case review study with the aim of furthering our knowledge of the topic.
Please cite this article as: Oliveri Aruete F, Candelario Cáceres A, Alonso Mallo E. Secuestro pulmonar intralobar bilateral en adulto joven. A propósito de un caso. Arch Bronconeumol. 2017;53:281–282.