Tuberculosis (TB) is a major health problem worldwide, and effective control remains a challenge. Risk is especially high for migrants due to the difficulties they may encounter in the host country: disrupted social networks, social exclusion, reduced accessibility to health care, lack of egalitarian participation in society, lack of trust, understanding or respect for the system.1 Portugal, with more than two million citizens living abroad, is the European Union country with the highest number of emigrants per capita.2
In order to characterize Portuguese emigrants diagnosed with TB when returning to their homeland, we performed a retrospective analysis of all such individuals diagnosed with TB in 2014 in Northern Portugal, evaluating both clinical and social-demographic data. New TB cases were identified from the national tuberculosis surveillance system and local TB centers were contacted for more detailed information. Continuous variables were described bymedian and interquartile range (25th–75th percentile) and categorical variables by relative frequencies (in percentage).
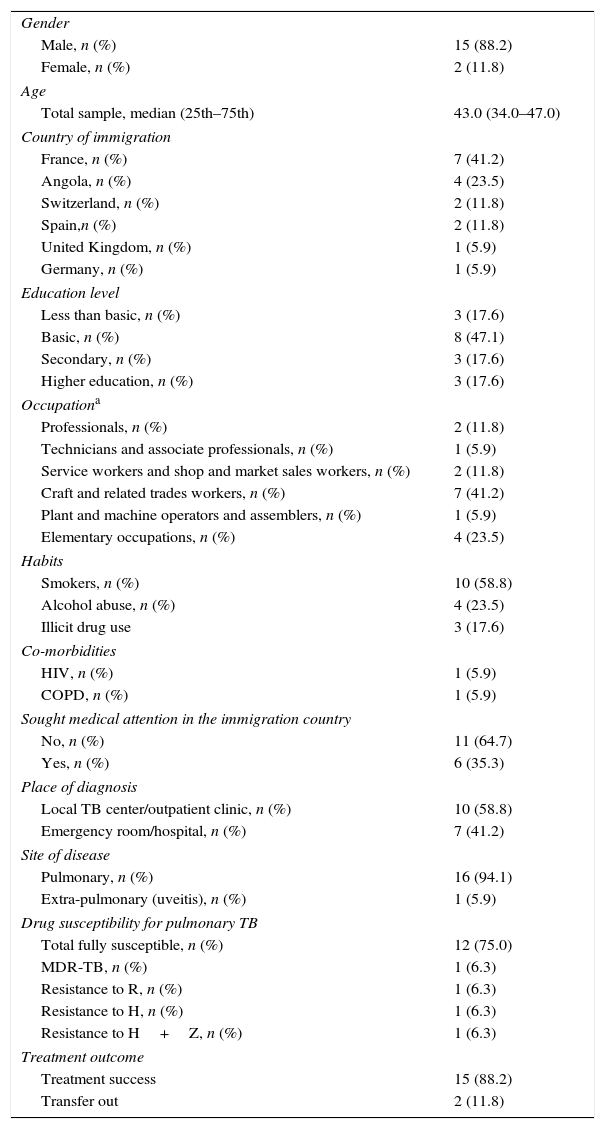
During the studied period, 17 returned Portuguese emigrants were diagnosed with TB in Northern Portugal. Socio-demographic, life-style and clinical characteristics are presented in Table 1. The median age at diagnosis was 43.0 years, and 88.2% of the patients were male. The majority of patients were immigrants in low-burden TB countries (n=13, 76.5%).3 Median residence in the host country was 42.0 months (4.3–138.0). The majority of patients worked in the construction industry (n=9, 52.9%). One patient was a health care worker. Fifty-three percent (n=9) of patients shared a house with non-family members, most of them sharing a room with another co-worker (n=6, 66.7%).
Socio-demographic, Life-style and Clinical Characteristics.
| Gender | |
| Male, n (%) | 15 (88.2) |
| Female, n (%) | 2 (11.8) |
| Age | |
| Total sample, median (25th–75th) | 43.0 (34.0–47.0) |
| Country of immigration | |
| France, n (%) | 7 (41.2) |
| Angola, n (%) | 4 (23.5) |
| Switzerland, n (%) | 2 (11.8) |
| Spain,n (%) | 2 (11.8) |
| United Kingdom, n (%) | 1 (5.9) |
| Germany, n (%) | 1 (5.9) |
| Education level | |
| Less than basic, n (%) | 3 (17.6) |
| Basic, n (%) | 8 (47.1) |
| Secondary, n (%) | 3 (17.6) |
| Higher education, n (%) | 3 (17.6) |
| Occupationa | |
| Professionals, n (%) | 2 (11.8) |
| Technicians and associate professionals, n (%) | 1 (5.9) |
| Service workers and shop and market sales workers, n (%) | 2 (11.8) |
| Craft and related trades workers, n (%) | 7 (41.2) |
| Plant and machine operators and assemblers, n (%) | 1 (5.9) |
| Elementary occupations, n (%) | 4 (23.5) |
| Habits | |
| Smokers, n (%) | 10 (58.8) |
| Alcohol abuse, n (%) | 4 (23.5) |
| Illicit drug use | 3 (17.6) |
| Co-morbidities | |
| HIV, n (%) | 1 (5.9) |
| COPD, n (%) | 1 (5.9) |
| Sought medical attention in the immigration country | |
| No, n (%) | 11 (64.7) |
| Yes, n (%) | 6 (35.3) |
| Place of diagnosis | |
| Local TB center/outpatient clinic, n (%) | 10 (58.8) |
| Emergency room/hospital, n (%) | 7 (41.2) |
| Site of disease | |
| Pulmonary, n (%) | 16 (94.1) |
| Extra-pulmonary (uveitis), n (%) | 1 (5.9) |
| Drug susceptibility for pulmonary TB | |
| Total fully susceptible, n (%) | 12 (75.0) |
| MDR-TB, n (%) | 1 (6.3) |
| Resistance to R, n (%) | 1 (6.3) |
| Resistance to H, n (%) | 1 (6.3) |
| Resistance to H+Z, n (%) | 1 (6.3) |
| Treatment outcome | |
| Treatment success | 15 (88.2) |
| Transfer out | 2 (11.8) |
The distribution of the occupation status is according to the major groups proposed by the International Standard Classification of Occupations – ISCO88.8
Abbreviation: COPD, chronic obstructive pulmonary disease; H, isoniazid; HI, human immunodeficiency virus; MDR-TB, multi-drug resistant tuberculosis; R, rifampicin; TB, tuberculosis; Z, pyrazinamide.
Recent exposure to pulmonary TB (previous 2 years) was reported by 3 patients (17.6%), 1 of whom reported exposure in Portugal to a close family member and 2 to a cohabitant member in Angola and France respectively. None of the 3 patients had undergone contact tracing or screening for TB. One patient reported a history of pulmonary TB. None of the patients were taking immunosuppressive drugs. Median time from symptom onset to diagnosis was 85.5 days (59.5–147.0) and from return to Portugal to diagnosis was 14.0 days (10.0–37.0). Six patients (35.3%) sought medical advice in their host country due to symptoms, but TB diagnosis was not suspected or pursued. Among patients who did not seek medical advice in their host country (n=11, 64.7%), 72.7% (n=8) were working in the construction industry and reported having been strongly advised to return to Portugal for medical advice by their employers. It was unclear whether this was due to their being in an illegal situation or if there were any other barriers to health care. All 16 patients with pulmonary TB had positive smear sputum at the time of diagnosis. The majority of patients reported multiple symptoms of tuberculosis: cough was the most frequently reported symptom (n=14, 82.4%) followed by night sweats (n=9, 52.9%) and weight loss (n=9, 52.9%).
This study characterizes returned Portuguese emigrants diagnosed with TB in their country of origin. Despite the limited number of patients, our findings give further insight into the challenge of effectively managing TB in migrant populations. Study subjects had resided in their host country for more than 2 years, on average, suggesting that exposure to TB probably occurred in that country. Three patients reported recent exposure to pulmonary TB, 2 of them in the host country and 1 in Portugal, and none of them were properly investigated. This situation raises some questions about the challenges surrounding contact tracing of TB patients abroad, and suggests that communication procedures between countries could be improved.
The median time between symptom onset and diagnosis observed in this study was 85.5 days, in line with some published data. In 1 study in a TB outpatient clinic in Northern Portugal in 2014, median time from onset of symptoms to diagnosis was 36 days,4 although national data from the same year report a median time of 104 days.5 In 2014, a total of 817 cases of TB were reported in the tuberculosis national surveillance system in northern Portugal, with a median time from onset of symptoms to diagnosis of 96 days in all cases. Data from France reported a median delay between symptoms and diagnosis of 97 days,6 and a systematic review found an average delay in TB diagnosis of 61 and 68 days in high-income and low-middle income countries, respectively.7
Another interesting finding in this report is the short interval (14 days) between return to Portugal and TB diagnosis. This suggests that once in Portugal, many patients sought medical advice as soon as possible, and were diagnosed in a short period of time. In fact, 64.7% of patients did not seek medical advice in their host country, despite the presence of symptoms.
Improved understanding of the barriers that migrants face in TB diagnosis is important from a perspective of worldwide management of the disease. This insight can also help each country optimize TB diagnosis in the migrant population and strengthen communication channels between countries.
Please cite this article as: Redondo MT, Carvalho C, Correia AM, Duarte R. Tuberculosis en los portugueses residentes en el extranjero. Arch Bronconeumol. 2017;53:279–280.