Tuberculosis (TB) is a highly prevalent disease in Peru.1 Lymph node involvement presents a particular challenge, as it is often difficult to diagnose, and treatments unsupported by scientific evidence may sometimes be prescribed, given that this entity can be confused with Kikuchi-Fujimoto disease (KFD).
We report the case of a 7-year-old boy from Lima, in his second year of primary school, who was referred to the respiratory medicine department by his pediatrician for left axillary lymph node enlargement, with no previous history of respiratory symptoms or fever. He had been fully vaccinated according the WHO vaccination schedule, which in Latin America includes Bacillus Calmette-Guérin (BCG). He had no history of previous TB, but his mother reported a possible exposure 6 months before the episode, when she took the child along to a prison to visit a family member who was an inmate there. The family member did not have a diagnosis of TB, but in Peru the high prevalence of this disease among the prison population means that visiting one of these establishments is considered a risk factor.
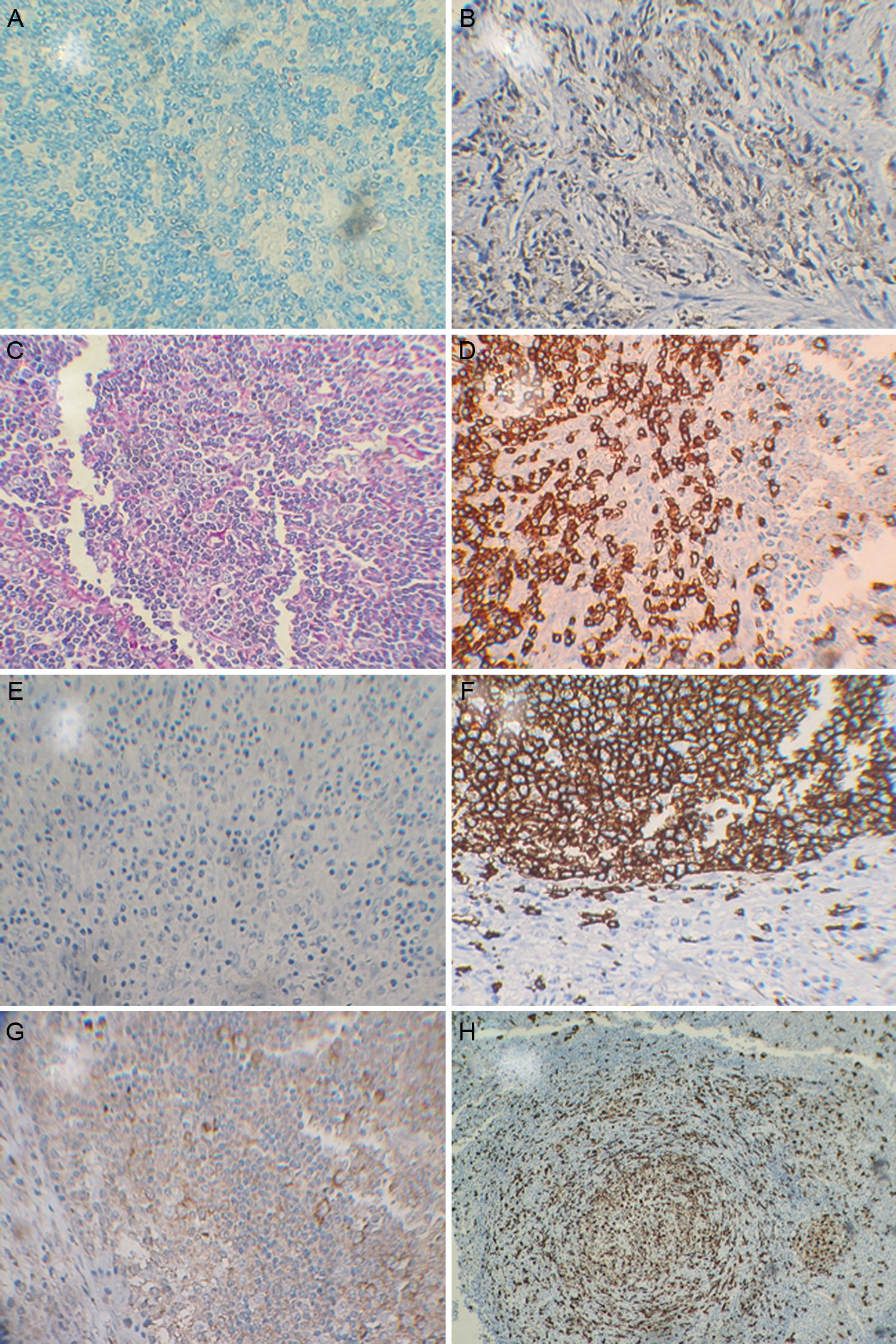
No respiratory abnormalities were found on examination, but painful lymphadenopathies measuring ±2cm were observed in the region of the left axilla. The rest of the examination was normal and no abnormalities were found on blood tests. Imaging studies revealed increased bronchovascular markings, with no pathological lesions on chest radiograph, and axillary lymphadenopathies measuring 2.2cm on ultrasonography. Sputum tuberculin testing (PPD) and sputum smear were negative for alcohol-acid resistant bacilli. A lymph node biopsy was performed, and the sample was sent for study. The biopsy was not cultured for Mycobacterium tuberculosis. After receiving the pathology study, which reported chronic, mildly granulomatous lymphadenitis, lymph node tuberculosis was considered as a first option, and admission to a TB program to start treatment was planned. However, as part of a special protocol, polymerase chain reaction (PCR) was performed on the lymph node biopsy for M. tuberculosis with sequence IS6110, with negative results. Samples were sent for immunohistochemistry testing, with the results shown in Fig. 1.
The patient was diagnosed with KFD and did not receive antituberculosis treatment. The clinical picture resolved after 3 weeks of symptomatic treatment.
Tuberculous cervical lymphadenitis is the most common manifestation of TB of the head and neck in our setting, and accounts for 15% of cases of extrapulmonary TB.2 Both tuberculous lymphadenitis and KFD are diseases that form part of the differential diagnosis of necrotizing lymphadenopathies.2–5 KFD is a rare disease that consists of histiocytic necrotizing lymphadenitis, and is generally self-limiting with a benign course. It affects mainly younger individuals, and is more common among females than males.3 Although it has been described mostly in Asian populations, cases have been reported worldwide. It generally presents in the form of enlarged, mainly unilateral cervical lymph nodes (70%–90%),5,6 accompanied in some cases by fever, fatigue, night sweats, and gastrointestinal and cutaneous changes.35,7,8 Laboratory and imaging data are not characteristic, so diagnosis can be difficult: a lymph node biopsy is required for correct identification, since fine needle aspirates tend to be inconclusive.6
Pathogenesis remains unclear to date, but some authors have suggested that both interferon and interleukin-6 (IL-6) or cell apoptosis may play some role, pointing toward viral5,9,10 or autoimmune9,11 etiologies. It seems clear that KFD is an exaggerated T cell-mediated reaction to a variety of mostly infectious stimuli.5,7,8,12 The course is usually benign, and it resolves in a few months without specific treatment, although some more severe cases have occasionally been reported.5,7,13
Histological findings correspond to 3 disease stages (proliferative, necrotizing and xanthomatous), representing progressive pathological changes.14 The typical immunophenotype of this disease consists a predominance of CD8+ cells over CD4+ T cells. Consistent immunohistochemistry results shows CD68 and CD3+, CD20+/− and CD30−. Histiocytes expressing myeloperoxidase and CD68 are characteristic of this disease.14
Chest radiograph must be obtained from all patients to rule out the possibility of other causes such as neoplasms or TB. Multislice spiral tomography is of particular use in locating the most accessible lymph node for biopsy and for determining the extent of the disease.6
In Peru, a country with a very high prevalence of TB, lymph node involvement is found in a good number of cases. Lymph node biopsy studies are included in diagnostic protocols, and epidemiological factors and other laboratory findings are taken into consideration. However, antituberculosis treatment is sometimes prescribed without hard scientific evidence and before the other etiological options, which would include KFD, have been explored. We therefore hold that is important to include this disease in the differential diagnosis of lymphadenopathies, particularly for lymph node TB, and appropriate studies must be conducted to avoid the prescription of costly drugs that might be unnecessary and carry significant risks for the patient.
We thank the professionals of the Hospital Nacional Arzobispo Loayza, and Drs. Alberto Yuen and Guillermo Ríos of the Laboratory of the Universidad Nacional Mayor de San Marcos, Lima, Peru, for their invaluable support.
Please cite this article as: Ching JNC. Enfermedad de Kikuchi-Fujimoto como diagnóstico diferencial de tuberculosis ganglionar. Reporte del primer caso de enfermedad de Kikuchi-Fujimoto en Perú. Arch Bronconeumol. 2017;53:282–284.