In the staging of lung cancer (LC), several tests are utilized. A computerized tomography (CT) and a positron emission tomography (PET) scans help determine size and extension of the tumor. However, tissue sampling is essential for an accurate diagnosis and therapeutic decision-making.
We present a case in which the therapeutic management and prognosis of a patient were significantly impacted by a broncho-echoendoscopy performed by a pulmonologist (EUS-B).
A 69-year-old active smoker woman was referred to the pulmonary department due to a lung nodule detected on a chest x-ray, requested for catarrhal symptoms.
A CT showed a left upper lobe mass (38mm×33mm). A PET revealed a maximum standard uptake volume value (SUVmax) of 16.63, while the SUVmax in the left adrenal gland (LAG) was 5.41. The nuclear medicine official report indicated a benign etiology rather than neoplastic in the gland. Although there are publications suggesting a lower SUVmax, a cut-off point of 6 is accepted as the threshold above which a malignancy is likely to be its cause.1
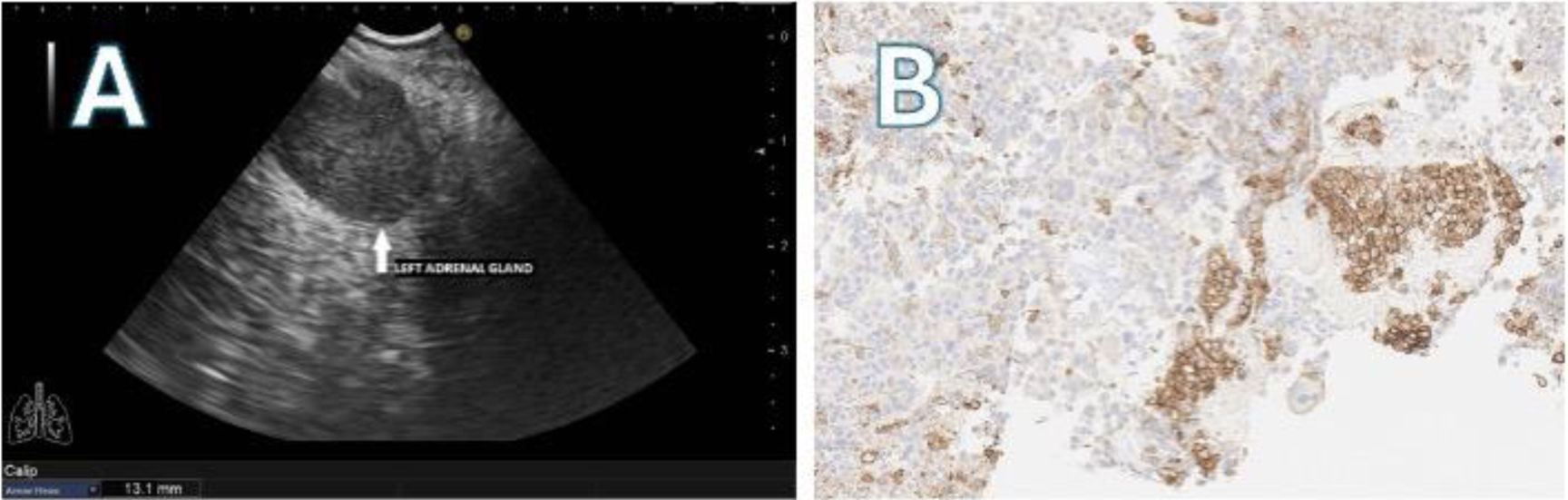
We performed a systematic echobronchoscopy. Three small 4L Lymph nodes (LN) were visualized and biopsied. Despite the PET report, we decided to perform an EUS-B through the esophagus using the same echobronchoscope (EB19-J10U, Pentax). A 13.1mm nodule was punctured in the LAG (Fig. 1A) using a 22G needle (SonoTip EBUS ProFlex, Medi-Globe). The procedure lasted for 20min, and no complications were encountered.
The pathological anatomy (PA) of the LAG biopsies was compatible with pulmonary adenocarcinoma metastasis. Molecular analysis was weakly positive for PD-L1 (<50%) (Fig. 1B). The mediastinal 4L LNs were negative for malignancy.
The tumor committees decided to perform an upper left lobectomy followed by a left adrenalectomy. Importantly, the LAG probably would not have been resected but for the diagnosis obtained with EUS-B.
The PA of the lung revealed adenocarcinoma. The analyzed LN (7-11L-12L) were negative for malignancy. The left adrenalectomy PA was consistent with metastasis from lung adenocarcinoma and showed the same PD-L1 levels as the EUS-B samples.
Based on the 8th edition of the TNM classification for LC in effect at the time of diagnosis, the pathologic stage was pT2cN0M1b.
One year after treatment, the patient shows no clinical or imaging evidence of tumor recurrence.
Performing EUS-B to combine mediastinal and extra-thoracic staging during a single endoscopy is feasible and safe2 and it is recommended by international guidelines. We have shown that the results obtained by pulmonologists are similar to those obtained by gastroenterologists.3
Adrenal metastases are present in 8% of stage IV LC. The presence of adrenal metastasis without LN involvement (skip metastasis), although less frequent, is associated with a better prognosis than those with LN involvement.4
It is important to confirm the location and number of extrathoracic metastasis, especially after the proposed changes in the new 9th edition of the TNM,5 as this has implications for the patient's prognosis and management.
In conclusion, EUS-B offers pulmonologists a valuable tool for the detection of malignant lesions in the upper esophago-gastric region in a single procedure. It can reduce the number of invasive procedures typically conducted in the staging of patients with suspected LC.
Authors’ contributionStudy concept and design, JCH; Drafting of the manuscript, JCH, LFF, FLG; Critical revision of the manuscript for important intellectual content, JCH, LFF, FLG.
Informed consentThe patient has signed the informed consent form.
Conflict of interestsThe authors state that they have no conflict of interests.
We would like to thank Bartolome Celli (Brigham and Women's Hospital, Harvard Medical School, Boston, USA) for his work as a scientific advisor.