Endobronchial ultrasound (EBUS) and cryobiopsy are two established procedures in Pulmonology. Recently, a new technique called Transbronchial Mediastinal Cryobiopsy (EBUS-TMC or CRYO-EBUS) has been developed, which combines the benefits of both procedures. This innovative technique allows for a more comprehensive study of the mediastinal and hilar lymph nodes, yielding larger and better-preserved tissue samples. As a result, it has significantly improved diagnostic accuracy for various conditions, including both malignant and benign disorders, particularly lymphoproliferative syndromes.1
In some patients, mediastinal lymph nodes are challenging to access through the airway, whether it be transtracheal or transbronchial. As a result, experienced digestive endoscopists and pulmonologists have turned to the esophageal approach, using a technique known as EUS-FNA (endoscopic ultrasound-fine needle aspiration).2 It is widely recognized that certain mediastinal lymph node stations, such as station paraesophageal and station ligamentum pulmonale, can only be reached through this approach. Furthermore, EUS allows adequate visualization of the subcarinal station and paratracheal stations, especially the left ones, sometimes even better than that offered by EBUS imaging. Additionally, endoscopic ultrasound using bronchoscope (EUS-B) allows access to lesions located in the left lobe of the liver and the left adrenal gland.3
Many studies suggest the use of a combination of EBUS and EUS-B to enhance the effectiveness of diagnosing mediastinal lesions. However, both techniques typically rely on fine needle aspiration (TBNA and FNA), which can result in inadequate or insufficient sample sizes for accurate histological diagnosis. The development of targeted oncological treatments, also known as personalized or precision medicine, has led to the need for additional measures to improve diagnostic outcomes and obtain enough material for further studies. In certain situations, factors such as morphology, lymph node location, or patient characteristics can pose challenges in mediastinal cryobiopsy sampling. However, the utilization of a transesophageal approach for cryobiopsy expands the potential for obtaining accurate diagnoses in cases where traditional methods may not be feasible. Recent studies on transesophageal mediastinal cryobiopsy have shown promising results, despite the limited number of cases. Our objective is to present a series of cases where EUS-guided transesophageal mediastinal cryobiopsy (EUS-TMC) was performed, and to analyze the yield in various disorders.
Between January and September of 2023, a total of 31 patients at three hospitals in Spain: The Regional University Hospital of Malaga, Central University Hospital of Oviedo (Asturias), and HLA La Vega Hospital (Murcia), with mediastinal lesions were included in the study. We realize EUS-B due to the impossibility of performing conventional EBUS either due to the lesion's location or the patient's characteristics. All procedures were performed by the same operators at each center. All patients provided written informed consent prior to bronchoscopy. Both EUS-FNA and EUS-TMC were performed in the same procedure, using a 22G needle (SonoTip TopGain; Medi-Globe, Rohrdorf, Germany) and a 1.1mm cryoprobe (Erbecryo 20403.401; Erbe, Tubingen, Germany) subsequently. During the procedure, oxygen arterial saturation, heart rate, blood pressure, and standard leads I, II, and III of the electrocardiogram were monitored. Both procedures were consecutively performed on the same mediastinal lesion. Rapid on-site evaluation (ROSE) was not always available. Pathologists received one sample identified as EUS-FNA and another as EUS-TMC.
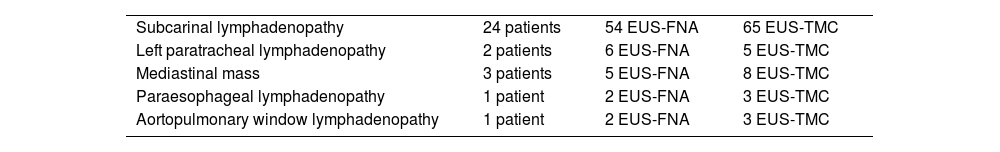
Of these, 71% were male with a mean age of 66.28±11.89 years. In 80.64% of cases, sedation was administered by the bronchoscopist. The most frequently used combination was midazolam with fentanyl, with average doses of 5±1.43mg and 56±12mg, respectively. Mediastinal lesions explored are listed in Table 1, with the most commonly biopsied being subcarinal lymphadenopathy. In terms of the lymph nodes’ ultrasound and morphological features, all were larger than one centimeter in their shortest dimension. Additionally, 71% displayed well-defined margins, 54.8% were uniformly echogenic, and 51.6% were lobulated. Out of the 10 lymph nodes, 5 were rounded and 5 were oval, with none showing a central hilar structure.
Mediastinal localization of EUS-FNA and EUS-TMC.
| Subcarinal lymphadenopathy | 24 patients | 54 EUS-FNA | 65 EUS-TMC |
| Left paratracheal lymphadenopathy | 2 patients | 6 EUS-FNA | 5 EUS-TMC |
| Mediastinal mass | 3 patients | 5 EUS-FNA | 8 EUS-TMC |
| Paraesophageal lymphadenopathy | 1 patient | 2 EUS-FNA | 3 EUS-TMC |
| Aortopulmonary window lymphadenopathy | 1 patient | 2 EUS-FNA | 3 EUS-TMC |
On average, 2.22±0.88 passes and 2.70±0.93 cryobiopsy samples were obtained, with EUS-FNA samples measuring 0.15±0.072cm and EUS-TMC samples measuring 0.44±0.12cm. A summary of these results can be found in Table 2. The diagnostic yield for EUS-FNA was 61%, while EUS-TMC had a 100% yield. However, the diagnostic concordance between the two techniques was only 42%. In 12 cases where EUS-FNA was inconclusive, a definitive diagnosis was achieved through cryobiopsy. Of these cases, 6 were determined to be neoplasms, 5 were negative, and one was non-necrotizing granulomatous disease. In instances where the final diagnosis was nonmalignant, patients were closely monitored for 6 months through clinical and radiological follow-up.
Results and diagnoses of EUS-FNA and EUS-TMC.
| Diagnoses | EUS-FNA | EUS-TMC |
|---|---|---|
| Cancer | 13 patients1 lymphoma12 lung cancer | 19 patients1 lymphoma16 lung cancer1 breast carcinoma metastasis1 colon neoplasm metastasis |
| Negative | 4 patients | 7 patients |
| Non-conclusive | 12 patients | 0 patients |
| Inflammatory | 2 patients2 sarcoidosis | 5 patients3 sarcoidosis2 reactive lymphadenitis |
In cases of neoplastic disease, EUS-FNA yielded 13 positive results (including one case of hematological disease), while EUS-TMC had a higher success rate with 19 positive results. Among these, 16 were diagnosed with lung cancer, while the remaining 2 cases were metastases from breast and colon carcinoma. Additionally, one case was identified as a hematological disease. The specific diagnoses are outlined in Table 2. Although most cases were benign, EUS-FNA revealed two cases of non-necrotizing granulomatous disease, while EUS-TMC identified five cases of inflammatory/reactive disease. Specifically, three cases were positive for non-necrotizing granulomatous disease and two for reactive histiocytosis. Our series of patients did not experience any complications during or within 24h after the procedure.
EBUS-TBNA is the technique of choice for mediastinal diagnosis. The combination with EUS-FNA allows for better sampling of lesions, given increased accessibility to all lymph nodes, particularly for neoplastic or benign disorders like sarcoidosis.4,5 Recently, transbronchial mediastinal cryobiopsy (EBUS-TMC) has been shown to obtain larger and more suitable samples, providing pathologists with better-preserved architecture, enabling multiple staining, immunohistochemical, and genetic-molecular studies and avoiding the need for repeat procedures.
Since 2013, there have been multiple publications on EBUS-TMC. One of the earliest studies6 focused on using a new cryo-needle to study mediastinal lesions in animals. Zhang et al.7 published the first series of patient cases in which they successfully performed an incision in the mucosa prior to inserting a cryoprobe, without any major complications. Despite this, there is a noticeable lack of literature on transesophageal access for cryobiopsy. However, Huang et al.8 in 2022 reported the first case of transesophageal mediastinal cryobiopsy, which yielded a positive result for lymphoma without any complications. In 2023, three cases were reported in our country. Salcedo et al.9 successfully performed the procedure on two patients under conscious sedation, resulting in positive outcomes for one lung cancer case and one inflammatory/reactive disease case. Another case, published by Ariza-Prota et al.,10 involved a patient with suspected lung cancer. In this case, a subcarinal lymphadenopathy was punctured and neoplastic cells were detected without any complications during the procedure.
A meta-analysis conducted by Botana et al. on 555 patients has shown an excellent overall diagnostic yield for EBUS-TMC. In our study, a diagnostic yield of 100% was achieved, significantly higher than the 12% yield reported for the transbronchial route.11 Maturu et al.12 focused on EBUS-TMC and examined cases where EBUS-TBNA did not yield conclusive results. Their research revealed a significantly higher diagnostic success rate of 59.3% with the addition of cryobiopsy. Our own series also encountered 12 non-conclusive EUS-FNA cases, which were successfully diagnosed through transesophageal cryobiopsy.
Transesophageal ultrasound-guided cryobiopsy is a valuable tool for diagnosing both neoplastic and benign conditions. Our case series has shown a higher success rate in detecting non-necrotizing granulomatous diseases compared to EUS-FNA. There were no significant complications during the procedure, unlike the complications reported in the literature when using the transbronchial route.
Conflict of interestsThe authors state that they have no conflict of interests.