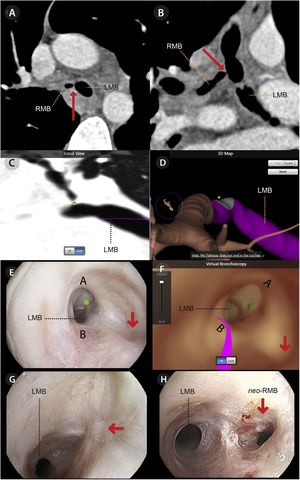
An 18-year-old lady with a history of pulmonary tuberculosis presented to us with recurrent pneumonia and reduced effort tolerance. CT thorax and bronchoscopy demonstrated a distorted trachea with multi-level tracheobronchial stenosis with no visualization of right main bronchus (RMB) ostium (Fig. 1A, B). Primary surgical repair was deemed high risk in view of the complexity of stenosis. Under rigid bronchoscopy, the site of RMB ostium was first postulated by observing the pattern of mucosal indentation and puckering but was proven inaccurate after verification by virtual bronchoscopic navigation (VBN, superDimension™, Medtronic, USA), Fig. 1C−F. After establishing a safety margin using convex probe endobronchial ultrasound at the proposed RMB ostium by VBN, the area of interest (Fig. 1G) was then punctured with a 20G transbronchial aspiration needle (TBNA) followed by passing of guidewire under fluoroscopic guidance. The puncture was successful after purulent secretion was seen flowing through the TBNA needle as well as swift advancement of guidewire into the right endobronchial tree. Mucosal incision was then performed with electrocautery knife in a radial manner. The incised ostium was then gradually dilated from 4 to 8mm employing the controlled radial expansion balloon. A 3.7mm slim bronchoscope was then able to be negotiated into the neo-RMB to allow airway examination and secretion clearance. The neo-RMB ostium was then treated with topical mitomycin C after bronchoscopic examination confirmed normal distal airway. As only a short segment of RMB was affected without bronchomalacia, we decided to adopt a watchful waiting strategy with mitomycin C application and an option to repeat balloon bronchoplasty rather than immediate stent deployment which itself may lead to further complications. Procedure was uncomplicated and RMB remain patent four months later (Fig. 1H) with significant improvement of total lung capacity from 2.36 to 3.63l.
Axial (Panel A) and coronal (Panel B) reconstruction of CT thorax showing RMB was occluded by a web-like structure (red arrow) with patent distal airways. The actual location of RMB ostium marked on VBN platform as a target (green dot) in Panel C and D. Correlation of bronchoscopic (Panel E) and virtual bronchoscopic images (Panel F) showing the postulated site of RMB ostium based on best-guess strategy (red arrow) and the actual site by virtual bronchoscopic navigation (green dot). The actual location of right main bronchus ostium identified by virtual bronchoscopic navigation pre-procedure showing subtle mucosal puckering with converging fibrotic bands (Panel G) and four months later which shown patent neo-RMB with minimal granulation tissue (Panel H).
Post-tuberculosis tracheobronchial stenosis (PTTS) is a debilitating and complex disease with multi-level airway involvement.1 To date, a standardized treatment strategy for PTTS has yet to be established. Although surgical reconstruction potentially offers a permanent solution for PTTS, it may not always be feasible in patients with poor respiratory reserve or when there is multi-level long segment stenosis.1 Thus, bronchoscopic approach maybe a reasonable up-front solution in patients with high surgical risk.2 For stenosis affecting the main bronchi with a visible ostium, multimodal bronchoscopic approach utilizing laser cauterization, electrocautery with balloon bronchoplasty is well described.3,4 However, in patients who present late with chronic total occlusion (CTO) of the main bronchi with no visible ostium, attempts to recanalize the airway are extremely challenging. Frequently, such patients will be managed conservatively if surgical reconstruction is deemed unsuitable. The most crucial step of recanalization is to locate the invisible ostium – although this can be postulated reasonably by observing the pattern of mucosal indentation and puckering, this may also be deceiving as PTTS frequently involves multiple areas in the central airway. This is illustrated in our case that the best-guess strategy was not always accurate and might carry the risk of creating a false track into the mediastinal structures. With the advancement of transbronchial access tools, a safe exit point from the airway can now be planned and localized safely with high confidence level.5 In essence, RMB-CTO as a result of PTTS is a complex condition with potential life debilitating consequences. Diligent pre-procedural planning and amalgamation of various interventional pulmonology techniques potentially offer a safe and novel approach into this century-old problem.