Diffuse alveolar hemorrhage (DAH) has a wide range of causes in children.1 Here, we present the first reported case of boy diagnosed with DAH due to bronchopulmonary dysplasia (BPD).
A 13-month-old male infant was transferred to our hospital for “recurrent pulmonary hemorrhage” with increased oxygen concentration supplement. The gestational age of the baby was 33+2wk. He presented postnatally with respiratory distress syndrome and underwent 13 months invasive mechanical ventilation (MV) because of severe BPD. On admission, he had tachypnea (56/min) with saturation at 92% on breathing machine (SIMV, PIP 23cmH2O, PEEP 9cmH2O, FiO2 80%). Moderate fine moist rales could be heard in both lungs. He has approximately 10ml fresh blood aspirated from the endotracheal tube per day.
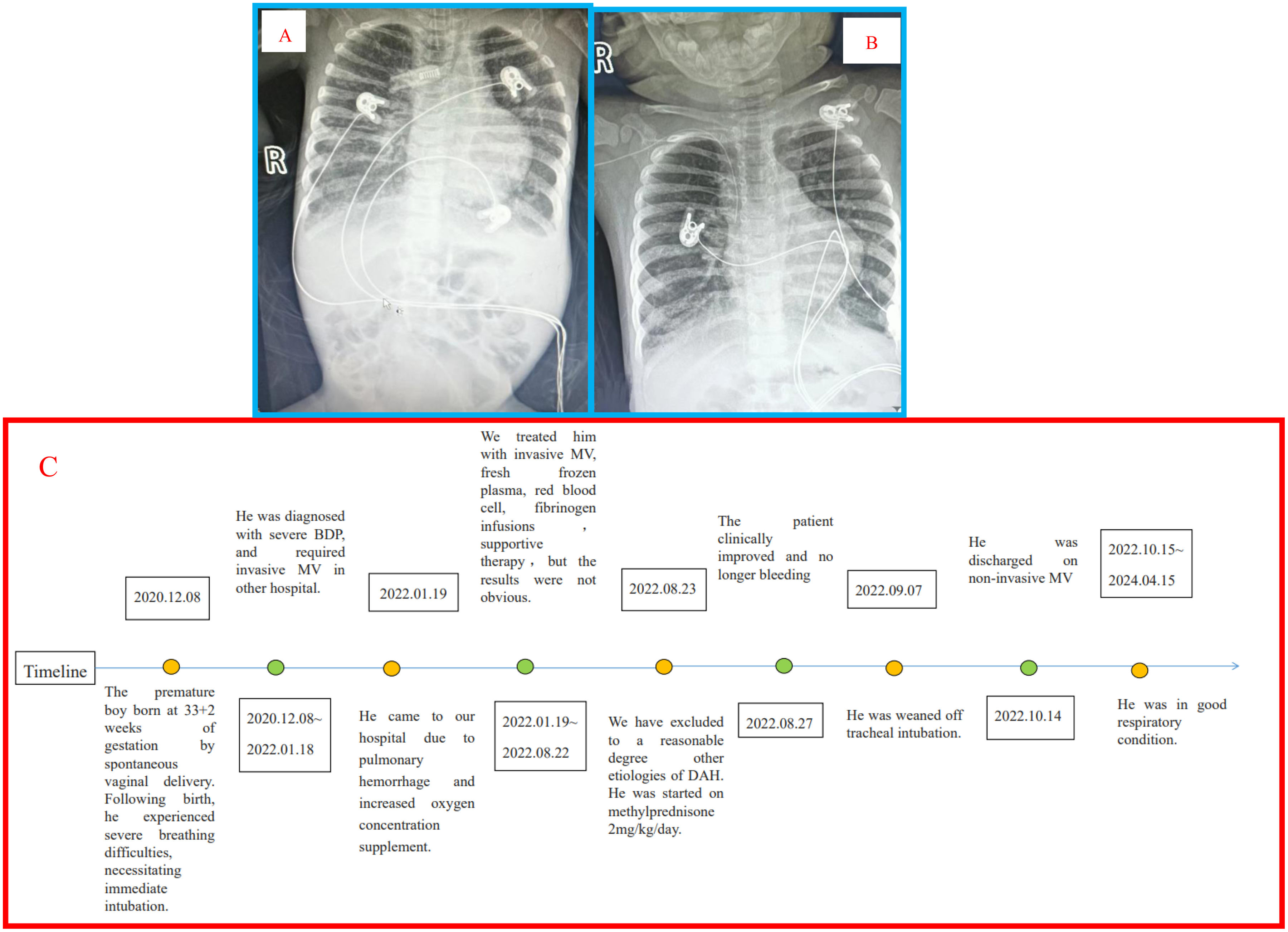
The test results, including biochemical examination, blood coagulation, platelet count, complement levels, ANA, ANCA, brain natriuretic peptide level, bacterial cultures of endotracheal aspirate, and gene test were unremarkable. Ultrasound showed normal LVEF and pulmonary arterial pressure. The bronchoscopy revealed progressively hemorrhagic effluent on bronchoalveolar lavage. Radiograph showed extensive consolidation in both lungs (Fig. 1A).
The patient was treated with invasive ventilator-assisted ventilation and oral methylprednisone at 2mg/kg/day with tapering for a total of 6 months. We adopted intermittent massage at the Hegu point to alleviate his discomfort, as this point can relief pain.2 Based on acupuncture treatment may improve lung function,3 he was given once acupuncture at the BL-13, EX-B1, BL-20, and ST-36 points. Interestingly, increased SpO2 were observed during the treatment. He was discharged on non-invasive ventilator support, had no further hemoptysis or dyspnea. His X-ray showed multiple mesh shadows in both lungs before discharge (Fig. 1B). After 1.5 years of follow-up, he was in good respiratory condition, without any cardiovascular complications or recurrent hemoptysis.
The boy experienced pulmonary hemorrhage 3 days before admission to our hospital, initially characterized by a daily volume of approximately 1ml, which progressively increased over time. The pathophysiology can be explained by the following reasons. Firstly, it is found that premature infants who died with BPD decreased expression of messages for vascular endothelial growth factor, which regulates endothelial cell migration and capillary permeability.4 Secondly, MV may destroy the pulmonary blood-gas barrier, which causes fluid, proteins, and blood cells to leak into tissues and air spaces.5
In recent years, acupuncture has increasingly being integrated into pediatric treatment, which has proven to be safe and effective.6 Based on the increased SpO2 in our study, we plan to explore acupuncture treatment for more children with BPD, a weak but positive recommendation can be made for the use of acupuncture in treating BPD.
The diagnosis of BPD for older gestational age infants is uncommon, but the patient had extensive imaging to assess his structural changes in the lungs. DAH as the progressive complication of BPD has not previously been described. This case demonstrates the need to increase the suspicion index of DAH in children with BPD, and highlight the favorable response to corticosteroid therapy in this vulnerable population.
CRediT Authorship Contribution StatementXiao-ying Zhao: Writing – review & editing, Writing – original draft, Formal analysis. Xiao-qi Zhang: Validation, Supervision. Guo-hui Kang: Validation, Methodology. Chang Chen: Methodology. Xin-ai Wang: Validation, Supervision. Wei Zheng: Methodology, Supervision. Jun Yuan: Supervision, Data curation, Conceptualization.
Declaration of Generative AI and AI-assisted Technologies in the Writing ProcessNo material in this manuscript has been produced with the help of any artificial intelligence software or tool.
FundingScientific research project of Hebei Province Administration of Traditional Chinese Medicine (2023320).
Conflicts of InterestThe authors declare no conflicts of interest.