Small cell lung cancer (SCLC) accounts for 15% of bronchial cancers.1,2 With its frequent bulky mediastinal involvement, SCLC can lead to central airway obstruction (CAO). Chemotherapy remains the upfront therapy in most cases given its rapid and major effect in this subtype of lung cancer.2 In cases of acute respiratory failure or obstructive pneumonia, where immediate action is required, therapeutic bronchoscopy (TB) can offer a rescue option to allow the patient to receive systemic treatments.3,4 Given this relatively rare occurrence, few studies have described the outcomes of TB in this population. Only two studies, one from Japan and one from Turkey, have published data specifically on SCLC patients undergoing TB for a total of 75 patients.3,4 Given this paucity of data, any further information on the outcomes of these patients could be useful for the management of these patients. In this context, our study aimed to describe French experience and outcomes of TB for SCLC using the EpiGETIF database.
The Groupe d’Endoscopie Thoracique et Interventionnel Francophone (GETIF), an entity created in 2001 regrouping 201 French speaking respirologists with an interest in interventional pulmonology, created the EpiGETIF registry in 2019, described in detail elsewhere.5 Its purpose is to gather exhaustive prospective multicenter data on endoscopic procedures, notably TB. Data on some important topics in TB have already been extracted from the database and published (or pending review).6–8 This article is part of this series.
This was a multicenter retrospective study involving all consecutive adult patients who underwent rigid TB for CAO caused by SCLC from January 2019 to May 2022 in 13 French hospitals. All TB interventions were performed under general anesthesia, in an operating room, using both a rigid bronchoscope and a flexible bronchoscope. The endoscopic technique was left at the discretion of the operator. CAO was defined as an obstruction of over 50% of the bronchial lumen and technical success as restoration of the patency of the targeted lumen over 50%. This study complies with MR-003 standards according to CNIL and the RGPD of the Assistance Publique-Hôpitaux de Marseille. Informed consent was obtained in accordance with national guidelines. Demographic, radiologic, bronchoscopic and follow-up data were entered prospectively by the local pulmonologists through the web-interface of the registry, using standardized definitions of each item. Pertinent missing data were recovered retrospectively by the investigators. EpiGETIF is a database created by the GETIF with the “Conseil National Professionnel (CNP)” of pulmonology, according to the 2019-17 governmental decree of January 9th 2019 relating to the missions of CNPs (CNIL number 2048574). Approval was obtained by the scientific committee of the registry to conduct the study. Statistical analyses were performed using Microsoft Excel software (Version 2002). Descriptive quantitative variables are presented as mean, standard deviation, median, 95% confidence interval and compared using the Student's t-test. Categorical variables are presented as frequencies (percentages). The alpha risk was set at 5%.
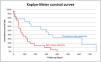
A total of 1934 TB were performed and entered in the EpiGETIF registry during the study period. Fifty-one of these cases (2.6%) were SCLC. All these patients were referred due to their respiratory symptoms, radiological findings, and endoscopy-proven endobronchial obstruction. Table 1 shows the patients’ demographic, clinical, radiological and procedural characteristics. Thirty-two patients (62.7%) had an Eastern Cooperative Oncology Group (ECOG) score of 2 or less. In 90% of cases, histology was known prior to the TB procedure and 48% of patients were naive to oncological treatment. Five patients were on mechanical ventilation (invasive or noninvasive). The mean dyspnea as assessed by a Borg scale was 6 before intervention with a mean decrease of 4 post intervention. Endoscopically, the obstruction involved the trachea in 20 patients (39.2%), the carina in 9 (17.6%) and one of the main bronchi in 38 (74.5%). The procedure was considered a complete technical success in 32 cases (62.7%), partial in 16 (31.4%), and unsuccessful in 2 cases (3.9%) (see definitions for partial and complete success in Ref. 5). In total, 38 stents were inserted in 34 patients (66.7%). Fifty percent were silicone stents and 52.6% were Y-shaped. Clinical improvement was noted in 82% of cases, allowing weaning of mechanical ventilation in most patients. There were complications in 16% of cases, essentially respiratory complications, with only 2 graded Clavien-Dindo 3 or higher, including 1 death. Survival data were available for 36 out of 51 patients. The median survival was 125, 299 and 67 days in the whole population, treatment-naive and previously treated patients, respectively (Fig. 1).
Characteristics of Patients, Radiology and Procedure.
| Characteristics (n=51) | n (%) or mean±SD |
|---|---|
| Patients | |
| Gender (female) | 21 (41.2) |
| Age, years | 63±8 |
| BMI, kg/m2 | 25.6±7.5 |
| Tobacco exposure, pack-years | 47±22 |
| Preprocedure WHO score | |
| 0 | 2 (3.9) |
| 1 | 17 (33.3) |
| 2 | 13 (25.5) |
| 3 | 16 (31.4) |
| 4 | 1 (2.0) |
| Oxygen support | |
| HFNC | 3 (5.9) |
| NIV | 1 (2.0) |
| MV | 4 (7.8) |
| Known histology prior to TB | 46 (90.2) |
| Radiology and endoscopy | |
| Obstruction type (per obstructed segment, n=83) | |
| Intrinsic | 15 (18.1) |
| Extrinsic | 24 (28.9) |
| Mixed | 44 (53.0) |
| Obstruction site (could be multi-level) | |
| Trachea | 20 (39.2) |
| Carina | 9 (17.6) |
| MSB | 38 (74.5) |
| BI or lobar | 16 (31.4) |
| Procedure | |
| Any stent inserted* | 34 (66.7) |
| Silicone | 19 (50.0) |
| Fully covered SEMS | 17 (44.7) |
| Partially covered SEMS | 2 (5.3) |
| Mechanical debulking | 26 (51.0) |
| Laser | 1 (2.0) |
| Electrocoagulation | 23 (45.1) |
| Balloon dilation | 8 (15.7) |
Percentages might not add up to 100% when data was missing.
Abbreviations: BI: bronchus intermedius, BMI: body mass index, HFNC: high-flow nasal cannula, MSB: main stem bronchus, MV: invasive mechanical ventilation, NIV: non invasive ventilation, SD: standard deviation, TB: therapeutic bronchoscopy, WHO: World Health Organization.
Despite the limitations of registry studies, there are valuable insights provided by this study. Comparisons with previously published contemporary data from this cohort can help distinguish SCLC patients undergoing TB compared to other types of MCAO.5 Unsurprisingly, the demographic data is comparable, except for more tobacco history in SCLC patients. The performance status (ECOG) distribution is also similar. The Borg score pre and post intervention suggests an immediate benefit in line with other types of cancer. The main difference we can outline is in the endobronchial presentation. There is a clear predominance of mixed and extrinsic obstruction over intrinsic obstruction in SCLC (81.9%) compared to other MCAO patients (56.7%). This is probably due to compression by bulky mediastinal lymph nodes. Correspondingly, we notice more stenting required in SCLC patients (66.7% versus 54.7%). However, stenting is a clinical decision based on the presence of a persistent significant obstruction following tumour debulking and the likelihood of response to future therapies and might vary between pulmonologists.
As mentioned earlier, chemotherapy with or without radiation therapy is considered the first-line therapy in SCLC.2 SCLC cases represented 2.6% of the total cohort of patients undergoing TB. This is lower than what is seen in the lung cancer population (around 15%) despite its propensity for mediastinal involvement and central airway obstruction.1,2,9 Interestingly, half of the patients received oncologic treatments before requiring TB. Also, more patients had an obstruction located at the trachea or main carina (56.9% versus 38.3%) and needed mechanical ventilation or high-flow nasal cannula than in the original cohort (15.7% versus 10.6%). Hence, it is likely that TB was used as expected as a salvage therapy when chemotherapy was deemed unlikely to be efficient (i.e. failed first-line) or contraindicated (i.e. obstructive pneumonia with sepsis or acute respiratory failure).
Unfortunately, missing survival data in our cohort mandates cautious conclusions on this topic. The median survival of 125 days in our study tends to be higher than in previous studies (37 and 47 days, respectively).3,4 The significant difference between previously treated and untreated patients is in line with what is expected of SCLC patients, given the gap in efficacy between first and other lines of treatment.2 The relatively low median survival of 67 days highlights the importance of tempering expected benefits of TB when discussing therapeutic options with previously treated patients. The treatments received after the procedure are unfortunately not entered into the registry and could not be recovered for most patients. It would have been interesting to know the rate of patients who could receive systemic treatment after TB, probably high given the relatively high median survival in this subpopulation (299 days).
In conclusion, the EpiGETIF registry has allowed the aggregation of data for specific subgroups of patients that are hard to study in single center case series. Though it is influenced by country-wide tendencies in training and availability of technologies and oncologic treatments, it is diverse and can inform clinicians on the efficacy of the invasive treatment they offer to their patients. In this subgroup analysis, we showed that SCLC who are selected to undergo TB for MCAO probably present more central airway involvement and need more stenting, but with clinical success similar to NSCLC patients from the same population.
Declaration of Generative AI and AI-assisted Technologies in the Writing ProcessAI was not used for the data analysis or writing of the manuscript.
FundingThe creation of the EpiGETIF registry has been partially funded by Novatech and PulmonX.
Conflict of InterestNone of the authors has any conflict of interest regarding this manuscript.