The antithyroid agents (carbimazole, methimazole, thiamazole, propylthiouracil and benzylthiouracile) are the drug class that is associated with a high risk of agranulocytosis. Isolated severe neutropenia or agranulocytosis, defined as an absolute neutrophil count of less than 0.5×109/L occurring in a subject treated with antithyroid agents should be considered as a drug-induced agranulocytosis, until proven otherwise. Agranulocytosis is rare and may develop in 0.2–0.5% patients using antithyroid drug therapy.1 The clinical evidence of infectious complications associated with antithyroid-drug-induced (ATD) agranulocytosis is usually symptomatology in fever (92%) and sore throat (85%), pharyngitis (46%), acute tonsillitis (38%), pneumonia (15%) and urinary tract infection (8%).2
A 61-year-old, Caucasian female was admitted to the emergency department with complaints with fever up to 39°C, chills and cough and general weaknesses which started a day after discharge from other hospital (hematology department) where she was treated for gastric pain and neutropenia (leukocyte was 1.2×109/L, neutrophils 0.03×109/L) induced by thiamazole. She was afebrile. Chest X ray was normal. She recovered successfully after 10th days with granulocyte colony-stimulating factor and discharged from hospital. Previously, she has been with hyperthyroidism for 21 years, six month ago before hospital admission her therapy was changed to thiamazole.
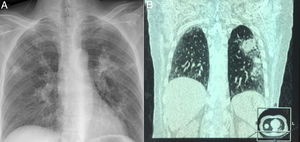
On admission to our hospital, her vital signs were within normal limits, except for a temperature of 38.8°C and respiratory rate 22/min. Physical examination revealed atonic bilateral equal air entry with no added rhonchi or wheezing. Cardiovascular and neurological examinations revealed no abnormalities. The abdomen was soft and non-tender, without palpable visceromegaly. Her initial chest X-ray showed a multifocal abscessing pneumonia (Fig. 1A). CT was immediately performed which confirmed multifocal abscessus in lungs (Fig. 1B). Admission labs revealed hemoglobin 12.5 gm/dL, white count 8.8×109/L, neutrophil 5.59×109, platelets count 197×109/L. Her serum sodium levels were 138mEq/dL, and the blood urea nitrogen (BUN) and creatinine values were 20mg/dL and 0.9mg/dL respectively. C reactive protein (CRP) was 252ng/ml, while procalcitonin was 78.7μg/L. Arterial blood gas showed a pH of 7.30 and PaO2 of 60mmHg, PCO2 46mmHg, SaO2 90%.
Initially, the patient was started empirically with broad-spectrum antibiotics: Vancomycin 1g/12h, Amikacin 1g/12g and Orvagyl 500mg/8h. Blood culture, throat culture, blood fungal culture, acid-fast bacillus blood culture, and urine culture were all negative. Despite antibiotics therapy, patient was febrile up to 38°C, and in the absence of adequate laboratory as well as radiologically answer, therapy was changed into Meropenem 1g/12h and Orvagyl 500mg/8h. On third day, patient was afebrile and feeling better. Her CRP was 9.7ng/ml, white count 11.2×109/L, platelets 210×109/L. During the following days, the patient's condition, and laboratory parameters improved in parallel with the neutrophil count. She received above mentioned therapy for fourteen days after she was discharged in good condition and radiological finding. She was released from the hospital with recommended Propylthiouracil 50mg twice daily. She was regularly checked up by endocrinologist and pulmonologist with no relapse of disease.
Antithyroid drugs, especially thioamides—including propylthiouracil, methimazole and carbimazole—have adverse hematological effects, ranging from mild leukopenia to agranulocytosis and aplastic anemia. Agranulocytosis, defined as a marked decrease in the number of granulocytes, frequently <500/μL, is a rare complication. Fever and sore throat are common symptoms of antithyroid drug induced agranulocytosis.3 Patients with an absolute neutrophil count <100/μL tend to have a greater risk of infectious and fatal complications than do patients with a neutrophil count >100/μL. The mortality rate is greater in patients aged ≥65 years than in those aged <65 years.4
The lungs are the most common organ to be infected in febrile neutropenic patients. The chest radiograph is the standard initial investigation to look for pulmonary changes, but its sensitivity has been shown to be very low. High resolution computed tomography (HRCT) chest can detect the abnormality with a high degree of accuracy, as well as differentiate between different types of infections.5 It is extremely useful in early detection or exclusion of a focus of infection and characterization of the focus. Exact etiological diagnosis is not possible in most of the cases, but identification of broad category of infective causes itself is very important for the appropriate therapy. Previous studies have proven that the most common cause of febrile condition is Pseudomonas aeruginosa.5 Our case was different from previous described in literature, in its beginning, but similar in good prognosis after granulocyte colony-stimulating factor and empirical antibiotic therapy. However, the recovery time in our cases was slightly longer than in previous cases (14 vs. 6.8 days).6 Nowadays, more people are undergoing surgical treatment as a permanent solution.7
In conclusion, ATD-induced agranulocytosis is rare, but the severity of this possibly life-threatening condition means its management is essential to a good prognosis. Our case suggests that patients with antithyroid drug-induced agranulocytosis who present with severe infections should be treated empirically with broad-spectrum antibiotics with antipseudomonal activity.
Alternative way in patients with hyperthyroidisms is surgery or radioactive iodine which seem to be effective options to restore an euthyroid state. In fact, radioactive iodine was demonstrated as a successful option, with 88.8% of patients experiencing euthyroidism after treatment.