The three basic types of congenital diaphragmatic hernia (CDH) include hiatus hernia, posterolateral Bochdalek hernia and anterior Morgagni hernia (MH), the last being the rarest type (2–3% of all cases).1,2 The diagnosis of MH in adults is very rare and usually is incidental or presents with non-specific chronic respiratory or gastrointestinal symptoms.2,3 It can also be present with acute bowel obstruction or intestinal strangulation.3 Late-presenting CDH is often difficult to diagnose, and delays in treatment are common.4 Few cases have been described in the literature.
A 64-year-old non-smoker caucasian woman, with previous diagnosis of morbid obesity (BMI of 50kg/m2), arterial hypertension, hypertensive heart disease, hypothyroidism and depression was first admitted to our department in 2007 with a one-month history of progressive exertional dyspnoea, paroxysmal nocturnal dyspnoea and lower limb oedema, with no other symptoms. There was no history of recent trauma or surgery.
On admission, she was started on non-invasive ventilation (NIV) for hypercapnic respiratory failure (pH 7.35, PaCO2 72.4 and PaO2 40.2mmHg). The initial chest radiographs showed an hypotransparency on the right pulmonary lower lobe. The chest CT scan identified a large Morgagni hernia on the right side, with the compromise of the right lung volume and contralateral mediastinal deviation, as well as signs of pulmonary hypertension. The echocardiogram confirmed mild pulmonary hypertension (PSAP 49mmHg). She was referred to Cardiothoracic Surgery but was refused because of her surgery-related risk. She was discharged on long-term supplemental oxygen therapy and domiciliary NIV. Between 2008 and 2012 she was admitted three times for decompensated hypercapnic respiratory failure and for oxygen and ventilatory parameters adjustment. Diaphragmatic hernia was also bigger on the chest radiographs. In 2013 she was admitted five times in the context of emesis and gastroparesis. Despite a significant weight loss (BMI 50 to 41kg/m2), she maintained the need for both long-term supplemental oxygen therapy and NIV. At that time her lung function test showed a moderately severe obstructive pattern (FVC 1.05mL (67%); FEV1 0.64mL (52%); FEV1/FVC ratio 61.14%; TLC 2.87mL (82%); RV 1.76mL (106%); ITGV 2.50 (112%)). A new CT scan showed increased volume of the Morgagni hernia, which contained part of the transverse colon, all the ascending colon, loops of ileum and distal jejunum, with the insinuation of gastric antrum, leading to passive atelectasis of the middle lobe and right lower lobe and deviation of the mediastinal structures to the left hemithorax.
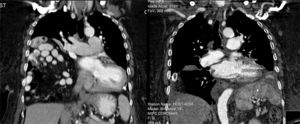
At the end of the year 2013, she was submitted to reduction and repair of the hernia and gastropexy, with a favourable expansion of the right lung (Fig. 1) and gradual resolution of global respiratory failure. Despite regaining weight (BMI 43kg/m2) it was possible to discontinue domiciliary NIV and supplemental oxygen therapy (pH 7.39, PaCO2 47.8 and PaO2 75.0mmHg in room air). The echocardiogram showed a reduction in PSAP from 49 to 39mmHg. There was a remarkable improvement in her lung volumes, that are now within the normal range (FVC 2.29mL (157%); FEV1 1.71mL (150%); FEV1/FVC ratio 74.75; TLC 4.47mL (127%); RV 2.01mL (117%); ITGV 2.45mL (110%)).
In 2014, she did a polysomnography which showed severe obstructive sleep apnea with a respiratory disturbance index (RDI) of 39.3/H and time oxygen saturation <90% (T90) of 19.9%. The patient was started on long-term positive airway pressure treatment with good adherence.
In our literature review, we could only find ten reported cases of MH with respiratory failure in adults.5,6 It is a rare aetiology for respiratory failure. It is usually asymptomatic or it presents with non-specific chronic symptoms. Because of these characteristics, the diagnosis of MH it is not often considered when changes in chest radiographs are present. Sometimes the typical radiological images of intra-thoracic gas-filled loops of the bowel are not present and it can appear as an opacity mimicking pneumonia, intrathoracic tumour, atelectasis, pericardial cyst or simulate a pneumothorax.3,4
Hypoventilation is a result of lung parenchyma compression by the abdominal viscera and diaphragm impairment, which causes a restrictive ventilatory defect.7 Oxygenation decreases due to alveolar collapse in the atelectatic lung.7 These changes in pulmonary mechanics and respiratory muscle performance tend to have worse outcomes in obese patients as they already breathe at abnormally low lung volumes. NIV is a useful tool as it improves alveolar recruitment of the affected area, while simultaneously increasing the functional residual capacity and minute ventilation.7 Nevertheless, NIV may also lead to deterioration of MH and consequently of respiratory status by causing aerophagia and abdominal distension.5 Another possible mechanism is by increasing intra-abdominal pressure when using high positive end-expiratory pressure.7 We think that in our patient the volume increase of the MH since 2007, when she was started on NIV, can potentially be explained by these mechanisms, complicated by the severe obesity.
On the other hand, there is no consensus or guidelines on surgical timing in non-acute cases. Although the majority of these hernias are asymptomatic, repair is recommended to avoid future complications2,3 and may improve lung function6 as we were able to demonstrate. Surgical intervention may also reverse chronic respiratory failure as Tone et al.5 report and we also found in this case. It is important to stress that the first lung function tests were carried out less than a month before surgery and that the patient regained weight after the surgical intervention. Another aspect to be mentioned is that our laboratory uses the ERS Quanjer 1993 lung function reference values8 which were validated to patients with a minimum height of 154cm tall. Since our patient height is only 141cm tall, her measured values as percent of predicted are globally overestimated and we should focus on the absolute volumes.
This case demonstrates the benefit of surgical reduction of this type of hernia, even in cases of chronic respiratory failure and additional causes for increased surgical risk.