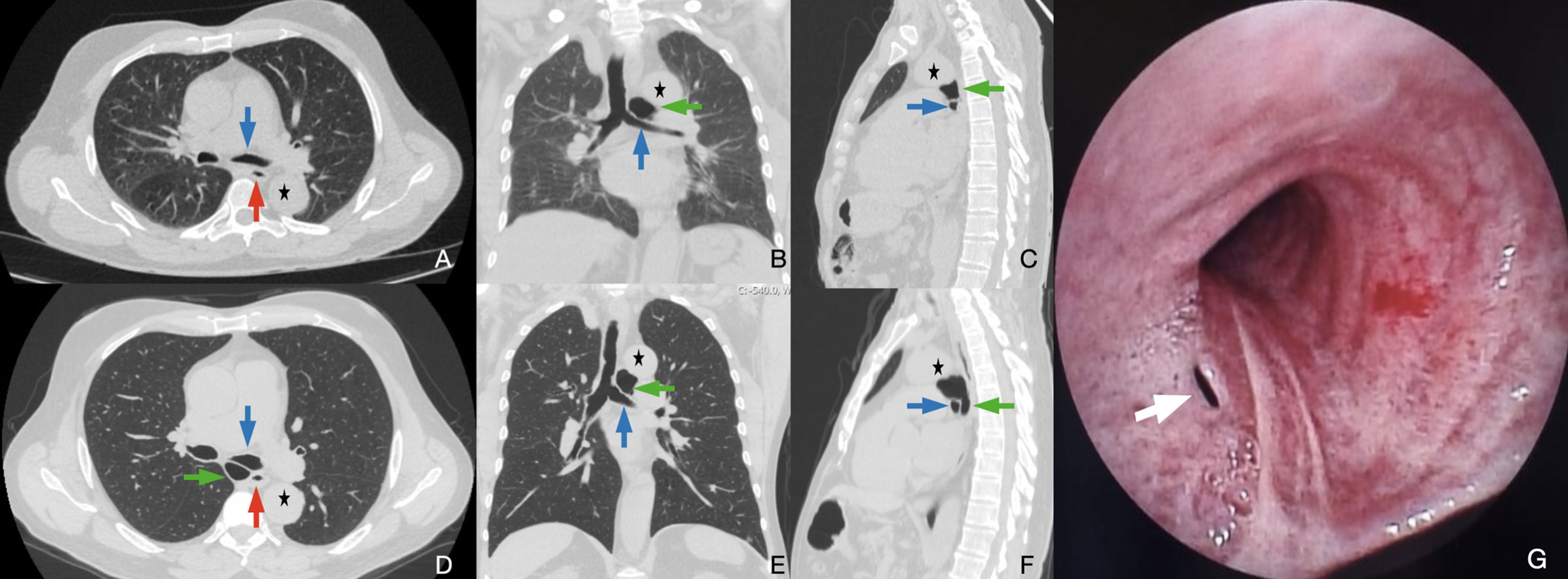
A 72-year-old male was recommended surgical resection for a bronchogenic cyst but declined, opting for conservative management with medical therapy and serial imaging. Initial computed tomography (CT) revealed a 28mm cystic lesion; follow-up four years later showed enlargement to 48mm with posterior extension into the subcarinal space (Fig. 1A–F). Fiberoptic bronchoscopy demonstrated smooth, non-obstructive compression of the posterior bronchial wall without mucosal invasion. A small mucosal defect was observed on the posterior distal trachea, suggestive of a fistulous communication between the airway and the cyst (Fig. 1G). This rare bronchoscopic finding likely represented a spontaneous tracheocystic fistula [1,2]. The tract may have functioned as a decompressive valve, allowing intermittent evacuation of cyst contents and ingress of air, thus explaining the paradoxical enlargement despite minimal symptoms [1]. The sequential images highlight progressive cyst growth and its evolving anatomical impact over time, underscoring the importance of long-term imaging in conservatively managed cases. While this tract may have alleviated pressure and reduced symptom burden, it also carries a potential risk of infection or acute expansion if obstructed. Given these findings, continued conservative management was pursued with close clinical and radiological monitoring.
Axial, coronal, sagittal CT, and bronchoscopic images demonstrating the progressive enlargement and airway involvement of a bronchogenic cyst over a four-year period. (A–C) Initial CT scans obtained four years earlier show a 28-mm cyst located superior to the left main bronchus, without significant airway compression. (D–F) Follow-up CT scans obtained four years later reveal enlargement to 48mm, with posterior extension into the subcarinal space and extrinsic compression of the left main bronchus. (G) Fiberoptic bronchoscopy image showing a small mucosal defect (white arrow) on the posterior wall of the distal trachea near the carina. The fistulous opening communicates with the bronchogenic cyst and exhibits visible air bubbles, consistent with a tracheocystic fistula. This rare finding supports a dynamic airway-cyst communication that may explain the paradoxical cyst enlargement during conservative follow-up. CT: computed tomography; Blue arrow: left main bronchus; red arrow: esophagus; green arrow: bronchogenic cyst; black asterisk: aorta.
This study was conducted ethically in accordance with the World Medical Association Declaration of Helsinki as revised in 1964. For studies with human subjects include the following: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Study approval statement: This study protocol was reviewed by the Scientific Research Ethics Committee of Recep Tayyip Erdogan University Faculty of Medicine, and an exemption was granted without requiring ethical approval.
Consent to publish statement: Written informed consent was obtained from the participant (or their parents/legal guardians/next-of-kin) for the publication of details of their medical case and accompanying images.
Author contributionsAuthor E.S.T., and O.T. have given substantial contributions to the literature search, data collection, study design, analysis of data, manuscript preparation, analysis interpretation of the data and review of manuscript. The illustrations belong to O.T. All authors have participated to drafting the manuscript, author E.S.T., and O.T. revised it critically. All authors read and approved the final version of the manuscript.
All authors contributed equally to the manuscript, read and approved the final version of the manuscript.
Artificial intelligence involvementWe declare that no material of the article has been generated in whole or in part from any artificial intelligence software.
Financial supportThe authors received no financial support for the research and/or authorship of this article.
Conflict of interestThe authors declare that they have no conflict of interest in the publication of this article.
Data availabilityThe data of this study were obtained from the patient database of Recep Tayyip Erdogan University Faculty of Medicine. The data can be shared if the corresponding author is reached via e-mail.
We would like to point out that we do not want an open access version and have transferred the copyright of the article to the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR).
The article has not been presented elsewhere and has not been reviewed by any other journal.
All the authors are aware of and approve the manuscript as submitted to this journal.