Obstructive sleep apnea (OSA) is a disorder characterised by partial or complete obstruction of the upper airway during sleep. It can lead to episodes of hypoxia, sleep fragmentation and changes in thoracic pressure. In the paediatric population, the prevalence of OSA is 1–4%, with a marked infradiagnosis.1 The leading cause of OSA in children is adenotonsillar hypertrophy, especially between the ages of 2 and 8 years. Other associated risk factors are craniofacial abnormalities, neuromuscular disturbances and obesity. OSA in the paediatric population is associated with morbidities such as neurocognitive and behavioural disorders, cardiovascular diseases, metabolic dysfunction and growth retardation with decreased quality of life.2 The index most commonly used to estimate the severity of the disease is the respiratory disturbance index (RDI) measured by polysomnography (PSG), but respiratory polygraphy has also emerged as a diagnostic tool in this population.3,4 In recent years, several studies have been conducted with the objective of validating the use of additional diagnostic tests, such as lateral neck X-ray, pulse oximetry, cardiorespiratory polygraphy and biomarkers (plasma and urinary), in order to speed up the diagnostic process.5
The most commonly used sleep questionnaire in the paediatric population is the Paediatric Sleep Questionnaire (PSQ), with a sensitivity and specificity of 85% and 87%, respectively. The PSQ was validated in patients aged between 2 and 18 years and has a reduced version of 22 questions and an extended version that assesses other non-respiratory sleep disorders. The questionnaire has 3 sections: nocturnal symptoms (A), diurnal symptom (B) and behaviour (C). Questions are simple and concise, with a response format of yes/no/don’t know, with the exception of items in the behaviour category in which 4 responses are available. Every question is scored from 0 to 1. The cutoff to indicate the presence of OSA is 0.33.6
The hypothesis of our study was that the PSQ would have good reliability with an area under the curve (AUC) significantly different from 50%. We conducted an observational, retrospective and single-centre diagnosis accuracy study with the aim of assessing the diagnostic value of PSQ for screening patients with suspected OSA. The study included patients aged between 2 and 16 years evaluated at the Sleep and Ventilation Unit for suspected OSA. Patients who were overweight, suffered from craniofacial malformations, Down's syndrome, neurological disorders, attention deficit hyperactivity disorder, patients undergoing a diagnostic study by polygraphy and patients with central apnea index≥3/h were excluded. The diagnosis was carried out by PSG with a minimum total sleep time of 180min to consider the validity of the study. The questionnaire was administered to parents on the night of the study. The receiver operating characteristic (ROC) curves of the test were constructed to evaluate the reliability of the scale and Youden's Index was calculated to assess the performance of the diagnostic test. The cut-off point of obstructive apnea–hypopnea index (AHIo)≥3/h was considered as a diagnosis of OSA following the recommendations of a Spanish consensus document.7 Patients were stratified according to AHIo (no OSA [AHIo<3/h], mild [AHIo: 3–5/h], moderate [AHIo: 5–10/h] and severe [AHIo: >10/h]) and according to age (children [from 2 year to 6 years], middle childhood [from 6 to 12 years] and teens [from 12 to 16 years]).
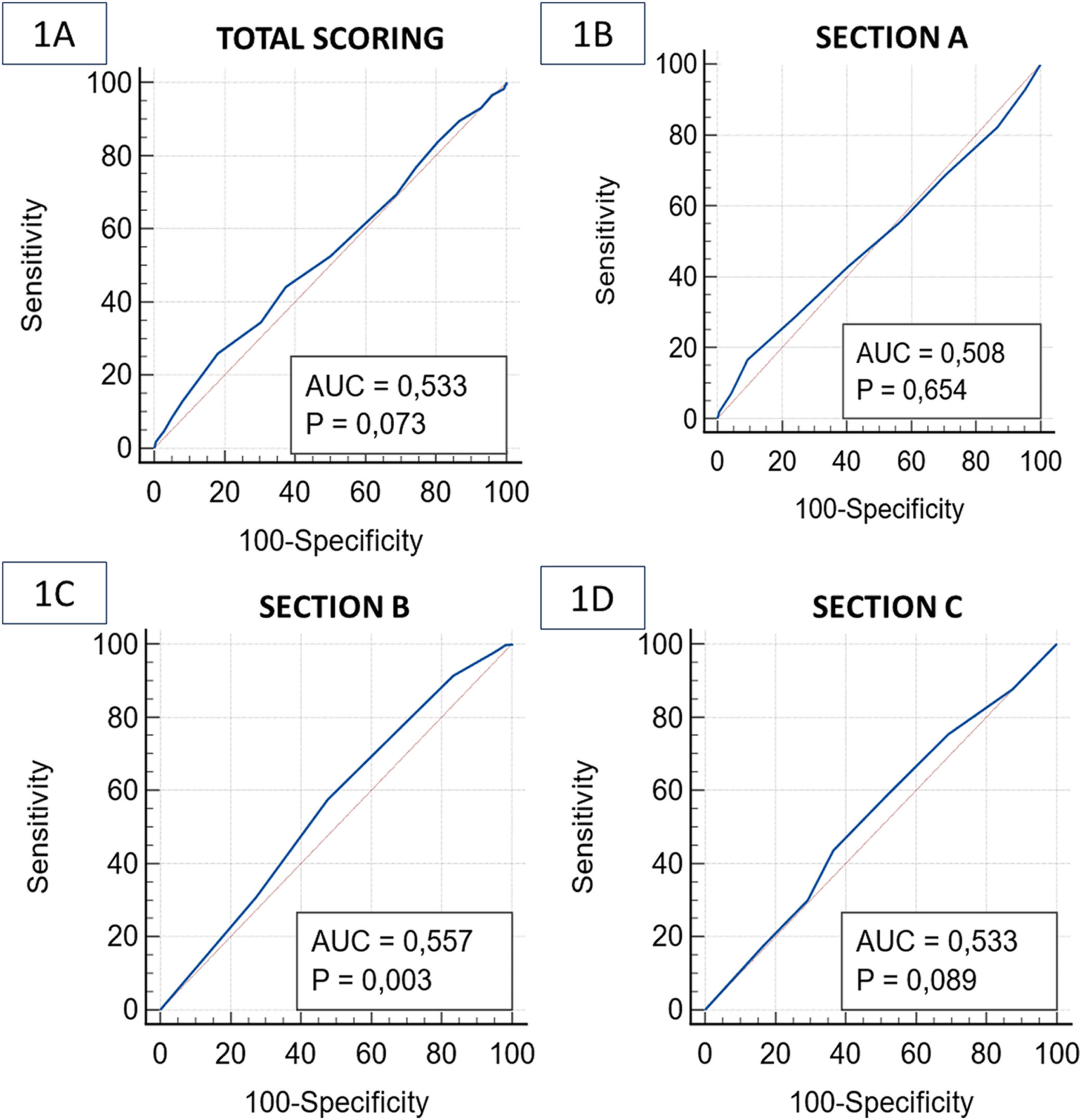
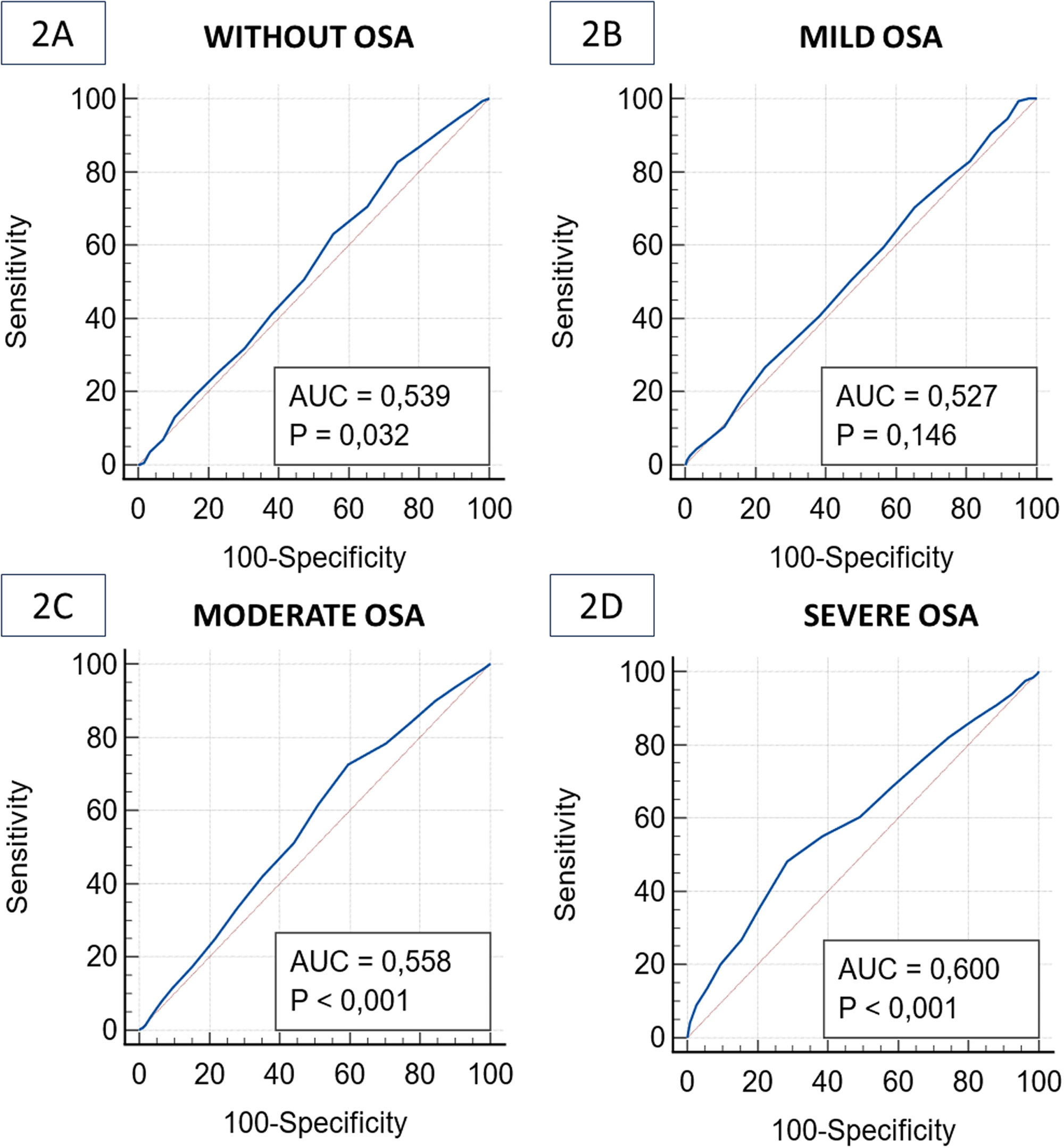
1482 patients were included in the study, 846 male (57.2%) and 634 female (42.8%), with a mean age of 10±3 years and a mean AHIo of 8.77±8.75/h. Diagnosis with OSA was established in 1203 patients (81.2%) (mild: 298, moderate: 519 and severe: 386). The area under the curve (AUC) for total scoring of PSQ was 0.53 (CI 95% [0.51–0.56], p=0.07). Youden's index was 0.07 and we obtained sensitivity of 52.45%, specificity of 49.82%, a positive predictive value (PPV) of 82% and a negative predictive value (NPV) of 19.4% (Fig. 1A). Producing the ROC curve by stratified sections of the questionnaire, there were no significant AUC results (Fig. 1B–D). In the AHIo analysis by subgroups, the AUC for patients without OSA (Fig. 2A) was 0.54 (CI 95% [0.51–0.56], p=0.03, Youden's index=0.09) with sensitivity and specificity of 50.67% and 52.7%, respectively. For patients with mild OSA (Fig. 2B), the AUC was 0.53 (CI 95% [0.50–0.55], p=0.15, Youden's index=0.05), with sensitivity of 50.54% and specificity of 52.61%. For patients with moderate OSA (Fig. 2C), the AUC was 0.56 (CI 95% [0.53–0.59], p<0.01, Youden's index=0.10) with sensitivity and specificity of 51.25% and 55.81%, respectively. For patients with severe OSA (Fig. 2D), the AUC was 0.60 (CI 95% [0.57–0.62], p<0.01, Youden's index=0.20, associated criterion≤6) with sensitivity of 60.36% and specificity of 50.91%. When producing the ROC curve by stratified AHIo and sections of the questionnaire, there were no significant AUC results. In terms of age subgroups, the AUC for the total PSQ score for children was 0.58 (CI 95% [0.55–0.60], p<0.01, Youden's index=0.14), for middle childhood it was 0.54 (CI 95% [0.51–0.57], p-value=0.01, Youden's index=0.07) and for teens it was 0.50 (CI 95% [0.47–0.54], p=0.82, Youden's index=0.02). When producing the ROC curve by stratified age and domains of the questionnaire, there were no significant AUC results. When comparing the relationship between the gender of the sample and the questionnaire score, there was no difference between the two genders in the total test score. When analysing by sections, women scored significantly higher in section B (p=0.015), while men scored significantly higher in section C (p=0.001).
(A) Receiver operating characteristic (ROC) curve with the area under the curve (AUC) of total scoring of Paediatric Sleep Questionnaire (PSQ). (B) ROC curve and AUC of scoring for section A of PSQ. (C) ROC curve and AUC of scoring for section B of PSQ. (D) ROC curve and AUC of scoring for section C of PSQ.
(A) ROC curve with the AUC of total scoring for PSQ in patients without obstructive sleep apnea (OSA). (B) ROC curve and AUC of total scoring for PSQ in patients with mild OSA. (C) ROC curve and AUC of total scoring for PSQ in patients with moderate OSA. (D) ROC curve and AUC of total scoring for PSQ in patients with severe OSA.
One of the most widely used screening tools for identifying children with OSA is the PSQ. The validation study of PSQ only analysed a population of 54 patients with confirmed OSA (mean rate of AHI 13.1+11.5 [0.1–59.3]) with a wide age range (2–18 years). In our case, we found that the total PSQ score and the scores for the three sections showed poor sensitivity and specificity in assessing the diagnosis and severity of the disease.
To our knowledge, our cohort is the largest in which the efficacy of PSQ has been tested. Other studies have evaluated the sensitivity and specificity of the questionnaire with variable results: Chervin et al.8 (n=105, sensitivity: 78%, specificity 72%) and a meta-analysis of 37 studies found sensitivity of 76% and specificity of 43%.9 In a recent study evaluating the PSQ's prediction of severity in 477 children referred for suspected OSA, it was reported that the questionnaire had no discriminative ability with an AUC CI that crossed 50% at all severities, similar to our results.10
The discrepancy in the results may be due to the fact that our study was designed to assess the applicability of the questionnaire in routine practice, whereas in the validation study it was applied to a population that had already been diagnosed with OSA. Another explanation is that the original validation study selected a population with predominantly severe OSA with a very wide AHI range (0.1–59.3a/h), whereas in our case the patients present a predominance of moderate OSA. Another possible justification for the results may be due to the use of a higher cut-off point to establish the diagnosis (AHI>5a/h) which can lead to the selection of patients with high severity of disease. In our study, we selected a population that is more representative of clinical practice (predominantly mild-moderate OSA), using a cut-off point based on the Spanish diagnostic guidelines. It should be noted that the high prevalence of OSA in our population may be due to a previous assessment by an otolaryngologist specialising in paediatric obstructive sleep apnoea.
Some limitations of the study were the exclusion of overweight children and the absence of oesophageal pressure measurement, in contrast to the original study, but this measurement is not routinely recommended. However, the study had several strengths, including a large number of patients with a diverse age range, polysomnography confirmation of the diagnosis for all patients, and the use of a cut-off point in accordance with the guidelines.
In conclusion, in our cohort, the PSQ questionnaire had low reliability for establishing the diagnosis and severity of the disease. Therefore, PSQ should not be used routinely in the assessment of suspected childhood OSA and other as OSA-18 could be used.11
FundingThis work has not received funding of any kind.
Authors’ contributionsConceptualization: TDT, IB and MG; Methodology: TDT, IB, EC, PM and MG; Software: IB and PM; Validation: TDT, IB, PM, EC, VE and MG; Formal analysis: TDT, IB, PM, EC, VE and MG; Investigation: TDT, IB, PM and MG; Resources: TDT, PM EC and MG; Data curation: IB and PM; Writing: TDT, IB, EC, VE and MG; Original draft preparation: TDT, IB, EC, VE and MG; Writing – review & editing: TDT, IB, EC, VE and MG; Supervision: TDT, IB, PM, EC, VE and MG; Project administration: TDT, IB and MG.
Conflicts of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.
Artificial intelligenceIn this article there is not an involvement of artificial intelligence.