We report a 23-year-old female, occasional smoker with no personal medical history of interest, who presented with fatigue, fever, and wet and productive cough, associated to left pleuritic chest pain in the previous 7 days. Her physical examination revealed tachypnea, tachycardia, and high temperature (39°C). Blood pressure and oxygen saturation with no supplementary oxygen were normal. At auscultation of the respiratory system, left basal vesicular breath was absent with amphoric breath sound.
As she arrived, blood tests were done, finding leucocytosis and elevation of D-dimer and C-reactive protein. Renal and hepatic function and ions were normal. X-rays were performed and showed a left basal condensation cavitated. Chest ultrasounds were done, dismissing pleural effusion.
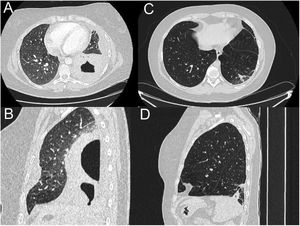
Since blood tests and X-rays were altered, a computed tomography (CT) pulmonary angiogram was performed (Fig. 1) to rule out pulmonary thromboembolism. Instead, an extensive consolidation that occupies the entire left lower lobe with two cavitations inside with air-fluid level was found, the largest one of 7cm. These findings suggested necrotizing pneumonia with lung abscesses (A and B).
CT pulmonary angiogram. Extensive consolidation that occupies the entire left lower lobe with two cavitations inside with air-fluid level, the largest of 7cm, suggesting necrotizing pneumonia with lung abscesses (A and B). Complete resolution of the pneumonic process visualizing in its place an area with fibro-atelectatic changes as a residual finding (C and D).
Microbiological examination for blood was positive for Dialister pneumosintes, even though she had neither personal history of oral infection nor dental manipulation. Sputum culture taken at her admission, viral serologies (HIV, HBV, etc.) and atypical bacterias study were negative. She received high dose of intravenous amoxicillin–clavulanate (2g every 8h for two weeks) and then changed to oral (maintaining same dose), completing 6 weeks of treatment. She also received respiratory physiotherapy during admission and at home.
The patient had a favorable clinical and radiological evolution and blood test became normal. Because of the excellent response to conservative treatment, we decided not to do bronchoscopy, balancing risk–benefits.
New thoracic computed tomography scan was done 4 months later, which showed consolidation and cavities resolution and residual fibrosis-atelectasis. Lung function tests were normal.
D. pneumosintes is an anaerobic, gram-negative, non-lactose-fermenting rod, belonging to normal bacterial flora of the oral cavity, pharynx, intestine, and vagina.1 It usually provokes soft tissue abscess or maxillofacial and periodontal infections.1,2 Nevertheless, its pulmonary infection is extremely rare, although there are some cases reported of mechanic-ventilated patients.3 There are no necrotizing pneumonia in an immunocompetent patient due to D. pneumosintes reported.
Necrotizing pneumonia is a severe and rare lung infection, which typical radiologic manifestation is as a gas-filled space within pulmonary consolidation, a mass, or a nodule.4 Usually, it has a subacute presentation, with wet and smelly cough, fever, and dyspnea.5
Its initial treatment is empiric antimicrobial therapy for oropharyngeal flora, being amoxicillin–clavulanate at high doses the elected antibiotic, to get into the cavitations. There is no agreement in the length of the treatment; however, at least should last from 4 to 8 weeks (the first 10–15 days parenterally), as we treated our patient. When conservative treatment does not work, it may be necessary CT-guided percutaneous drainage, and in rare occasions surgery is needed.5
Conflict of interestsThe authors state that they have no conflict of interests.