A 67-year-old patient, with a history of high blood pressure, presented with dyspnea on minimal exertion for 1 month and required 2 hospital admissions for respiratory infections.
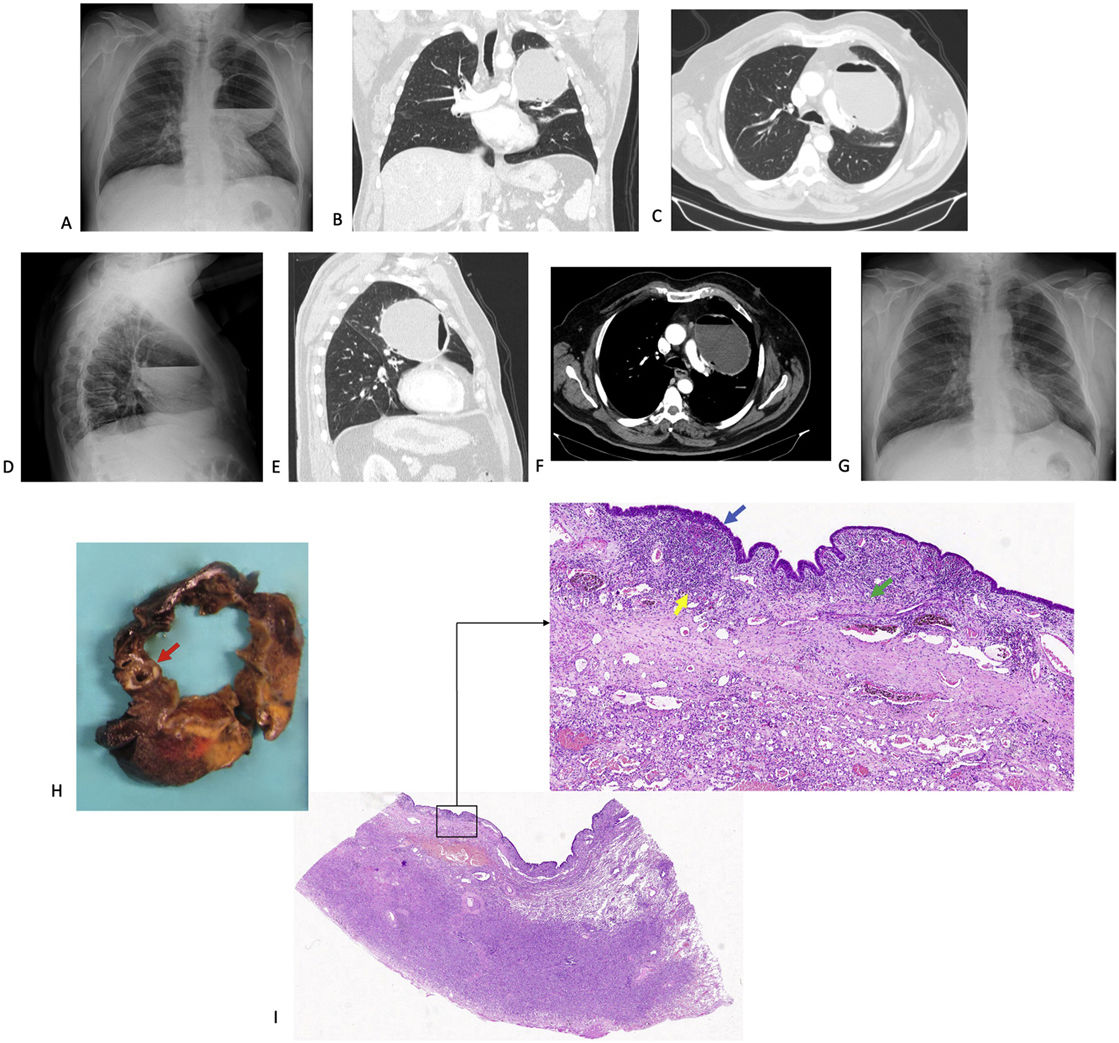
The chest X-ray (CXR) showed a voluminous cystic formation in the left hemithorax with air-fluid level content (Fig. 1). In the computed tomography (CT), a thin-walled cystic formation with air–fluid level content measuring 118mm×90mm×85mm is observed, which has extensive contact with the mediastinal pleura and bronchovascular structures of the hilum, displacing the anterior segmental bronchus of the left upper lobe (LUL) and its artery, considering the possible diagnoses of pneumatocele versus bronchogenic cyst. In bronchoscopy, there were no endobronchial lesions.
(A) Voluminous cystic formation with air-fluid level content that occupies more than 1/3 of the left hemithorax in the posteroanterior projection of the chest X-ray; (B) CT scan coronal plane, showing the displacement and compression of vascular structures due to the pulmonary cystic lesion; (C) CT scan axial plane at the level of T6; (D) lateral projection of the chest X-ray; (E) CT scan sagittal plane; (F) CT scan axial plane in soft tissue window; (G) chest X-ray performed 5 months after surgery; (H) in the segmentectomy specimen, a unilocular cystic cavity with a maximum diameter of 65mm was recognized, which was focally in connection with a bronchus (red arrow); (I) this cavity was lined by bronchial respiratory type epithelium (blue arrow), with residual smooth muscle fibers (green arrow) and marked underlying chronic inflammation (yellow arrow), characteristic findings of cystic bronchiectasis.
Given the clinical and radiological and intraoperative findings, left apical tri-segmentectomy was performed by video-assisted thoracoscopic surgery (VATS), without incident.
The pathology showed a cystic bronchiectasis with severe chronic inflammation and acute abscessed inflammation. In the surrounding parenchyma there was fibrosis, histiocytic alveolar desquamation and foci of organizing pneumonia.
In the radiological tests, the differential diagnosis of large solitary pulmonary cystic lesions may include hydatid cyst, giant bulla, pneumatocele, pulmonary sequestration, congenital lobar emphysema, congenital pulmonary airway malformation (CPAM), bronchogenic cyst and cystic bronchiectasis,1,2 as is our case.
To date, very few cases of large cystic bronchiectasis in adults have been reported2 and, apparently, this is the first documented case that has been treated by anatomical pulmonary sublobar resection by VATS.
Conflict of InterestsThe authors declare that they have no conflict of interest related directly or indirectly to the contents of the manuscript.