In all health systems around the world, intensive care unit (ICU) beds are essential1. Nowadays, we are facing an aging population, and it has been estimated that in 2050 in Europe, the percentage of the population that will be 80 years old or older will represent nearly 10%, and only with these patients will comprise 10–20% of all ICU admissions2. It is important to be prepared for this situation, being necessary to innovate in medical technology and establish standard care procedures.3,4
In adult patients connected to mechanical ventilation (MV), tracheal suctioning is a common care realized by nursing personnel. This procedure consists of inserting the probe of an open suction system (OSS) or closed suction system (CSS) through the endotracheal tube to remove secretions to avoid discomfort and occlusion of the airway.5 Tracheal suctioning practices can increase the rates of cross-contamination that triggers ventilator-associated pneumonia (VAP).6 VAP is defined as pneumonia that develops in an intubated patient after 48h or more of MV support.6,7 VAP has an impact on morbidity, days of stay in ICU (up to 13 days more), treatment (more antibiotics), and mortality (increases by 9.4%).8,9
CSS is the gold standard for tracheal suctioning in many countries, but COVID-19 caused an increase in their use in those countries where CSS was still not used.10 However, there is still no clear evidence that the benefits outweigh the risks using CSSs. It is obvious that it can be used to control patients with contagious diseases. In these cases, it is important its use as protection for health personnel.10 However, there are still many variables and relevant aspects that must be analyzed.
This study aimed to explore the evidence surrounding the two different methods for tracheal aspiration to determine if CSS has better results than OSS in adult patients connected to MV, due to it is not yet as explored field.
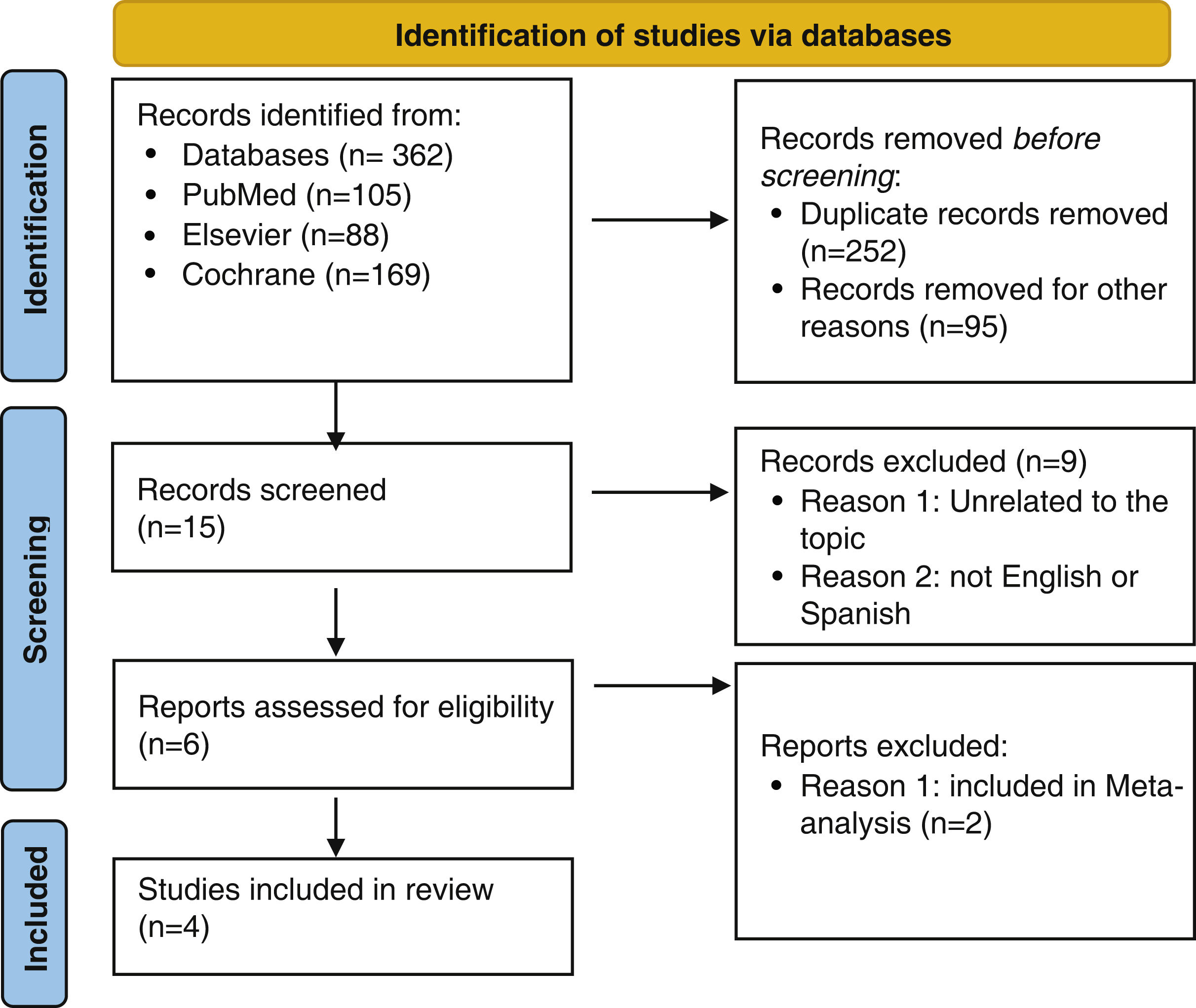
We conducted a systematic review registered in The International Prospective Register of Systematic Reviews (PROSPERO) (CRD42023401103). All eligible primary research studies and literature reviews containing outcomes of bacterial colonization of tracheal aspiration with a CSS in patients connected to mechanical ventilation admitted to an ICU were included. The tracheal suction included was both emergency and programmed. Only articles published with free full text in English or Spanish were included in the review (Fig. 1). A total of four studies were included in the review (Table 1).
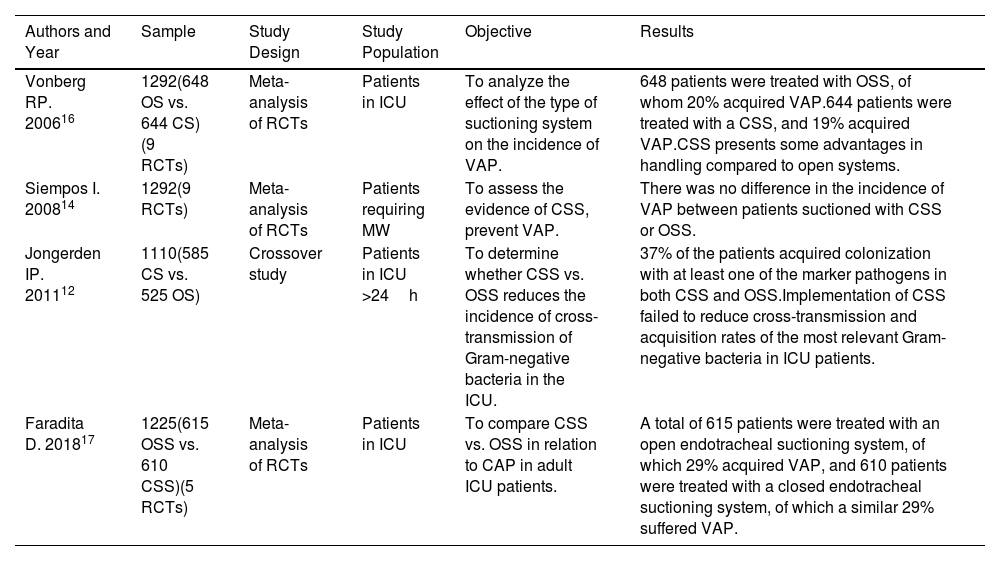
Selected Articles.
| Authors and Year | Sample | Study Design | Study Population | Objective | Results |
|---|---|---|---|---|---|
| Vonberg RP. 200616 | 1292(648 OS vs. 644 CS)(9 RCTs) | Meta-analysis of RCTs | Patients in ICU | To analyze the effect of the type of suctioning system on the incidence of VAP. | 648 patients were treated with OSS, of whom 20% acquired VAP.644 patients were treated with a CSS, and 19% acquired VAP.CSS presents some advantages in handling compared to open systems. |
| Siempos I. 200814 | 1292(9 RCTs) | Meta-analysis of RCTs | Patients requiring MW | To assess the evidence of CSS, prevent VAP. | There was no difference in the incidence of VAP between patients suctioned with CSS or OSS. |
| Jongerden IP. 201112 | 1110(585 CS vs. 525 OS) | Crossover study | Patients in ICU >24h | To determine whether CSS vs. OSS reduces the incidence of cross-transmission of Gram-negative bacteria in the ICU. | 37% of the patients acquired colonization with at least one of the marker pathogens in both CSS and OSS.Implementation of CSS failed to reduce cross-transmission and acquisition rates of the most relevant Gram-negative bacteria in ICU patients. |
| Faradita D. 201817 | 1225(615 OSS vs. 610 CSS)(5 RCTs) | Meta-analysis of RCTs | Patients in ICU | To compare CSS vs. OSS in relation to CAP in adult ICU patients. | A total of 615 patients were treated with an open endotracheal suctioning system, of which 29% acquired VAP, and 610 patients were treated with a closed endotracheal suctioning system, of which a similar 29% suffered VAP. |
Abbreviations: CSS: closed suctioning system; ICU: intensive care unit; MV: mechanical ventilation; OS: opening suctioning system; RCT: randomized controlled-trial; VAP: ventilator-associated pneumonia.
Regarding the antibiotics use, Jongerden et al.6 found that 75% of the patients with CSS were treated with antibiotics, while 73% of patients with OSS. In both groups, patients with CSS and patients with OSS, the most common antibiotic density was in penicilin-like antibiotics and cephalosporins. Rabitsch et al.7 did not found significant differences in antibiotic patterns between groups.
Jongerden et al.6 found Pseudomonas aeruginosa, Acinetobacter species, or Enterobacter species in 58% of the patients with CSS, compared to 60% of the patients with OSS. In patients with CSS, P. aeruginosa and Enterobacter species appeared less frequently (10.3 vs. 15.7 and 0.2 vs. 1.0) but the presence of Acinetobacter species was higher (2.7 vs. 0.4). The overall acquisition was 35.5 and 32.5 per 1000 patient-days during CSS and OSS, respectively. However, Siempos et al.8 included research that found significant differences in colonization rates between groups related to P. aeruginosa (p=0.01) and Acinetobacter species (p<0.01) that were more frequent in CSS than in the OSS.
Siempos et al.8 included research from Rabitsch et al.7 found significant differences between groups. Five cross-contaminations occurred in the patients with OSS but not in the patients with CSS. The cross-contamination occurred from bronchial to gastric juice in either direction. The cultures showed Candida albicans, Enterococcus faecalis, and Candida tropicalis cross-contamination.
Siempos et al.8 included research from Lorente et al.9 did not found significant differences between groups with CSS and OSS, but P. aeruginosa, Enterobacter species, and Serratia marcescens were more frequent in patients with CSS. Haemophilus species were more frequent in the group with OSS. They detailed the bacteria that developed VAP. The microorganisms appeared equal in patients with CSS and OSS; the most common were the Gram-negative bacteria, non-fermentative Gram-negative bacteria, Staphylococcus aureus, and Gram-positive cocci, respectively.
According to the cross-contamination, the incidence of VAP found by Lorente et al.9 was observed in patients with OSS and cross-contamination. Vonberg et al.10 found less risk ratio (RR) of VAP using CSS in six of the nine studies included, but these studies did not show significant differences. However, other studies have not found differences in the incidence density of VAP.8,9,11
This review provides conflicting results around bacterial colonization in adult patients connected to MV. The absolute recommendation of the use of CSS in all ICU patients connected to MV cannot be generalized.
Bardi et al.12 in 2021 found pneumonia appeared in 23% of critically ill patients, Johnstone et al.13 in 2023 showed the associated mortality of VAP at around 30–36%; therefore, there is an urgent need to strengthen the surveillance of patients with mechanical ventilation. For example, the risk of death increased with P. aeruginosa (OR 1.39 [95% CI, 1.05–1.83])14 and Acinetobacter species (OR, 1.40 [95% CI, 1.08–1.81).15
Nursing personnel must be careful when using OSS and CSS. Cobley et al.16 in 1991 showed that the potential advantages of CSS would be related to the maintenance of ventilator parameters. Yazdannik17 in 2013 said that it had not found significant differences in the reduction of contamination with potentially infectious organisms, but currently there is no clear evidence either.
Nowadays, we can only suggest the use of CSS in cases of respiratory infections like SARS-CoV-2 that could be spread from person to person primarily through large-particle respiratory droplet transmission and patient with a high risk of de-recruitment.18
In addition, the future of research could be related to new concepts like multidrug-resistant bacteria and their influence,19 probiotics for preventing VAP20 and other important aspects of ICU patients like nutrition, designed with a randomized clinical trial.
There is a necessity to update the use of CSS vs. OSS marking differences between patient and health care institutions, including patient variables such as cross-contamination, VAP, cardiorespiratory variables, and organization variables such as training, cost-effectiveness use, occlusion of endotracheal tubes, and environmental contamination. This type of research would be led by a multidisciplinary team because there are many professionals involved in tracheal suctioning.
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of InterestNone declared.
University of La Rioja.