Primary pulmonary angiosarcoma (PPA) is a rare malignancy that is often detected as advanced stage due to limited knowledge and most of the time misdiagnosed.1 In order to draw attention to this rare malignancy, we wanted to share our case with a diagnosis of endobronchial PPA mimicking asthma.
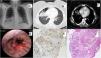
A 43 years old female patient was consulted due to radiological abnormality during preoperative evaluation of surgery for meniscal tear. The patient had shortness of breath and chest pain especially with exertion. She had been using different inhalers and antibiotic treatments intermittently for asthma-like symptoms for about 1 year and her chest X-ray was normal on initial addmission. Thorax CT was requested due to increased opacity in the lower right zone of the chest X-ray of the preoperative evaluation (Fig. 1A). CT imaging revealed a pneumothorax measuring approximately 4cm in the right hemithorax and a lesion 2.5cm in diameter causing obliteration in the middle lobe, lower lobe bronchus were detected (Fig. 1B and C).
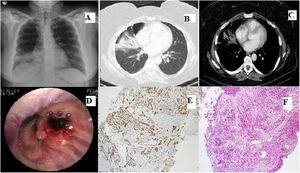
(A) Radiograph showing increased opacity in the right lower zone. (B and C) CT scan showing the mass and pneumothorax area. (D) Groups of neoplastic cells lined with atypical neoplastic cells with vasoformative properties, showing infiltrative growth through normal structures (H&E, 100×). (E) Malignant endothelial cells showing positive staining with CD31 (100×).
PET CT showed FDG uptake of the lesion and right hilar and paratracheal lymph nodes.
In bronchoscopy, it was observed that the right middle and lower lobes were narrowed; there was an endobronchial lesion and mucosal tumor infiltration at the entrance of lower lobe, and multiple biopsies were taken from this endonbronchial lesion (Fig. 1D).
In the bronchoscopic biopsy specimen, numerous irregularly shaped anastomotic vascular channels, a highly infiltrative architecture and a tumoral lesion covered with atypical cells with weak borders were observed (Fig. 1E). These cells showed diffuse strong positive staining with CD31, CD34, ERG (Fig. 1F) and vimentin. Negative reaction was observed with TTF-1, p40, pancytokeratin, EMA, S100, SOX10. With these findings, was reported as angiosarcoma.
Malignant involvement in 4R and 10R lymph nodes was demonstrated by mediastinoscopy. The patient was referred to medical oncology for chemotherapy.
PPA is a rare type of sarcoma with an aggressive course and generally poor prognosis. Angiosarcomas account for approximately 1–2% of all sarcomas.2 PPA is very rare and approximately 30–35 cases of PPA have been reported in the literature so far.2,3 It is commonly misdiagnosed due to nonspecific radiologic and bronchoscopic findings, common clinical manifestations mimicking other common lung diseases, and there are not specific diagnostic criteria. Although it is estimated to be more frequent in middle-aged and elderly males, our patient was a young female patient. While most of the PPA cases present with hemoptysis secondary to alveolar hemorrhage, our patient had dyspnea and chest pain. Most of the patients diagnosed with PPA were diagnosed with surgical procedure or autopsy data and 2 cases diagnosed bronchoscopically were detected in the literature. The detection of a pneumothorax area in the immediate vicinity of the lesion in ourpatient is similar to a case in the literature and suggests that angiosarcomas may cause this condition during progression.4,5
In conclusion, PPA, a rare malignancy, may localize endobronchially and mimic airway disease. Although the radiological examination is normal at the first admission, additional diagnostic procedures should be planned in patients who do not respond to treatment, and bronchoscopic examination should be performed for possible endobronchial pathologies in patients with persistent airway diseases.
Conflicts of InterestThe authors state that they have no conflict of interests.