Spontaneous pneumothorax occurring during pregnancy is an exceedingly rare condition, with fewer than 100 cases documented.1 Analysis of these rare instances affords several insights into therapeutic strategies for mitigating maternal–fetal risk.
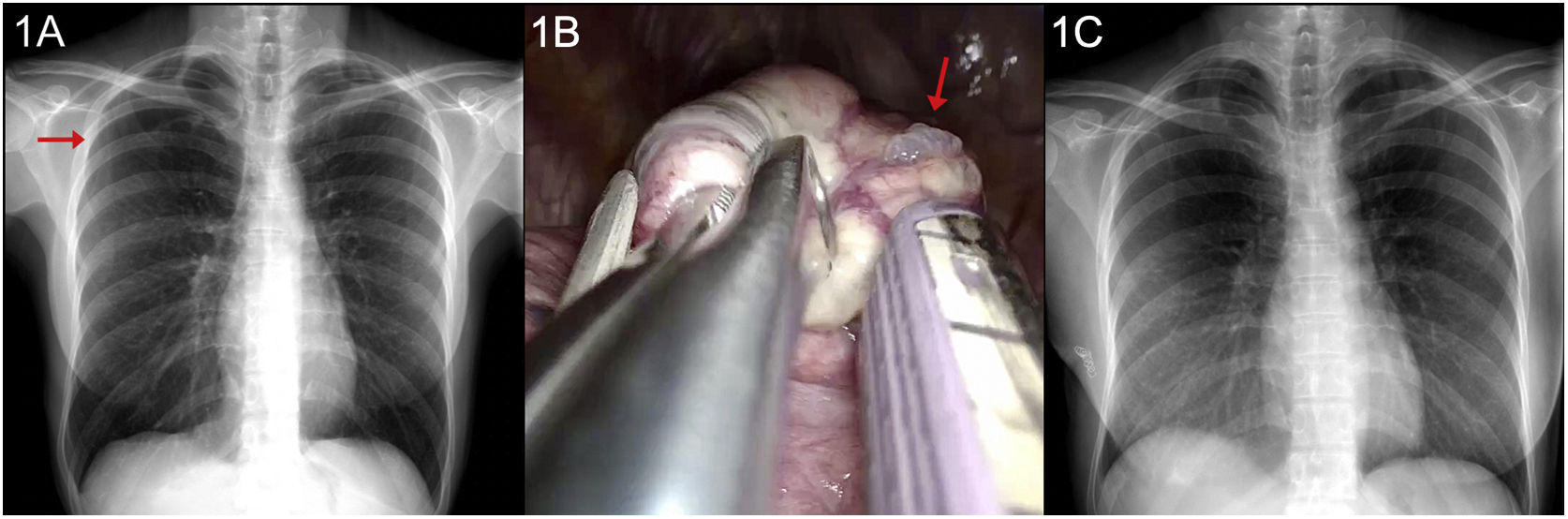
We describe the case of a 32-year-old non-smoking patient, who at 13 weeks gestation (WG), presented to the emergency department with symptoms of pleuritic pain in the right hemithorax. Her medical history included a spontaneous right-sided pneumothorax managed conservatively the preceding year. Initial examination found her hemodynamically stable, SpO2 97%. Further examination revealed diminished vesicular breath sounds at the right apex. Chest radiography, conducted with abdominal shielding, confirmed a diagnosis of partial right pneumothorax (Fig. 1A).
(A) Chest X-ray showing the presence of a right apical pneumothorax (red arrow). (B) Intraoperative image: Dystrophic/bullous complex observed in the right apical lung parenchyma (red arrow) and the stapler used for its surgical resection. (C) Postoperative follow-up chest X-ray shows no evidence of complications.
The patient was admitted for ongoing clinical and radiological surveillance. Given that the degree of lung collapse was at the threshold for pleural drainage placement, the decision was made for conservative management. After a 72-h hospital stay, the patient was discharged following radiological control showing no progression. A follow-up chest X-ray was performed at 3 weeks to confirm resolution of the pneumothorax. A multidisciplinary team involving the departments of Gynecology and Obstetrics and Anesthesia subsequently scheduled an elective surgical procedure for the second trimester.
During the 21 WG, the patient underwent right uniportal video-assisted thoracoscopic surgery (VATS) following the standard technique with a port at the level of the 4th intercostal space. The procedure involved performing a bullectomy and mechanical pleurodesis involving resection of the dystrophic/bullous right apical lung parenchyma (Fig. 1B). Her postoperative course was uneventful, leading to a discharge from hospital after 72h (Fig. 1C).
At 35 WG, the patient was diagnosed with preterm premature rupture of membranes. Labor was induced using oxytocin with a successful dilation completed under epidural anesthesia. Delivery was uncomplicated, resulting in the birth of a healthy male infant. The postpartum period was without any signs of pneumothorax or other complications. A thoracic ultrasound evaluation was performed to rule out the presence of pneumothorax in the peripartum period, specifically after labor. At a 6-month follow-up, the patient remained asymptomatic with no signs of recurrent pneumothorax.
Spontaneous pneumothorax should be considered as a differential in all pregnant women presenting with chest pain and/or dyspnea. Chest radiography, when performed with abdominal protection, serves as a safe diagnostic tool. Management of spontaneous pneumothorax during pregnancy, labor, or postpartum generally follows the same principles as for non-pregnant individuals. A conservative approach can be employed in the context of small pneumothorax (<2cm) in the absence of dyspnea or fetal distress.
The second trimester is considered optimal for surgical intervention, with organogenesis having completed and the risk of preterm labor being comparatively lower than at later gestational stages. VATS is the preferred surgical approach, with mechanical pleurodesis recommended.2
In most cases, spontaneous vaginal delivery at or near term, facilitated by regional anesthesia, is the preferred technique as it reduces strain during the second stage of labor. Cesarean section should be reserved for cases with obstetric indications.3
In conclusion, women with a history of spontaneous pneumothorax planning a pregnancy and who have not had definitive surgical treatment should be counseled on the risk of recurrence. The therapeutic plan and role of surgical intervention should be determined through a multidisciplinary discussion. Each patient's treatment strategy should be optimally tailored to their individual case.
Conflict of interestsThe authors state that they have no conflict of interests.