The outbreak of coronavirus disease (COVID-19) caused by severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), emerged in China in late 2019 and was declared a pandemic by the World Health Organization on March 11, 2020. By May 4, 215 countries had already been affected, and more than 3 million cases had been confirmed worldwide.1 This virus, a member of the Coronaviridae family, uses a spike protein to enter into the cell by binding to the angiotensin-converting enzyme 2 expressed in nasal, oral, lung, and colon cells, amongst other tissues.2
To address this global emergency and facilitate the overall management of this pandemic, the scientific community and health professionals are working on the development of new treatments and technologies to enable early diagnosis. The role of chest imaging, specifically radiography (X-ray) and computed tomography (CT), in the management of patients with suspected COVID-19 should be established taking into account factors such as respiratory disease severity, pretest probability of the disease, and the availability of resources.3
Currently, neither X-ray nor CT are recommended diagnostic criteria for COVID-19. The only accepted diagnostic method is viral screening, with the limitation that quantitative PCR results are only available after 6–48 h. Therefore, although viral testing is still required even when radiological findings are consistent with the disease, radiological imaging findings should be taken into consideration to establish a suspected diagnosis aimed at providing a more efficient triage not only involves screening of patients but also decision like quarantine the patients, admit them etc.3,4
Most publications support the accuracy of CT in detecting viral pneumonia, even in asymptomatic patients.5 In patients with a high clinical probability of COVID-19 who are positive on CT but with a negative PCR test, this imaging technique can be viewed as a screening tool, and a repeat PCR is indicated.6 The characteristic radiological findings of COVID-19 on CT include multiple peripheral pulmonary opacities, with frequent bilateral involvement, distributed predominantly in basal and posterior regions. X-ray reveals similar characteristics, but the sensitivity of CT is superior.7–10
No uniform criteria are available to guide the radiological evaluation of viral pneumonia in the context of a pandemic. The choice of imaging techniques is based not only on the properties of imaging techniques themselves, but also on the resources of the hospital, the availability of viral testing, expertise, and ultimately depends on the judgement of the team of professionals directly involved in the management of these patients.3
Digital tomosynthesis (DTS) of the chest is a technique that provides multiple anatomical images in a single scan. DTS shares some CT advantages and, although less sensitive, requires a lower dose of radiation (CT vs. DTS, 49×), and reduces costs. Aditionally, it alsohas several advantages over chest X-ray: 1) it improves lesion detection by reducing artifacts caused by overlapping anatomical structures; 2) it facilitates 3-dimensional localization; 3) it offers improved contrast resolution; and 4) it is more sensitive.11–15
DTS consists of a conventional X-ray tube, the movements of which are controlled from the console, a detector panel and reconstruction algorithms that produce tomographic images.
Up to 60 low-dose exposures are obtained during each pass. The data acquired are reconstructed in a group of coronal images of the chest, parallel to the detector plane, which can be reviewed sequentially in DICOM format on any standard workstation connected to the PACS. All DTS include a conventional PA projection in addition to the tomograms.
The role of digital tomography in the assessment of infectious lung disease is not yet established, although its efficacy in detecting pulmonary nodules and screening for breast cancer has been described.12,13
In our radiology department, DTS has been proposed as a preferred initial imaging technique for evaluating acute respiratory disease in patients with suspected COVID-19. To date, 62% of patients admitted with COVID-19 confirmed by quantitative PCR (n = 97; 56 men and 41 women) had baseline DTS, and the remaining 38%, who presented a worse clinical condition underwent chest X-ray. When the DTS radiological reports were classified according to the probability of COVID-19 as: 1) low; 2) intermediate; 3) high; or 4) no radiological alterations, we found that the results of 53% of the DTS performed prior to viral testing were highly probable and only 6% were normal.
In total, 13% of PCR-positive patients were admitted after their second DTS because they did not initially meet clinical admission criteria. In all cases, progressive pulmonary opacities were observed on DTS, in addition to worsening symptoms and clinical laboratory markers. Four cases were reported as low probability in the first DTS and high probability in the second; 2 patients had normal initial DTS and high probability in the second; and another 2 cases were reported as low probability in the first DTS and intermediate probability in the second.
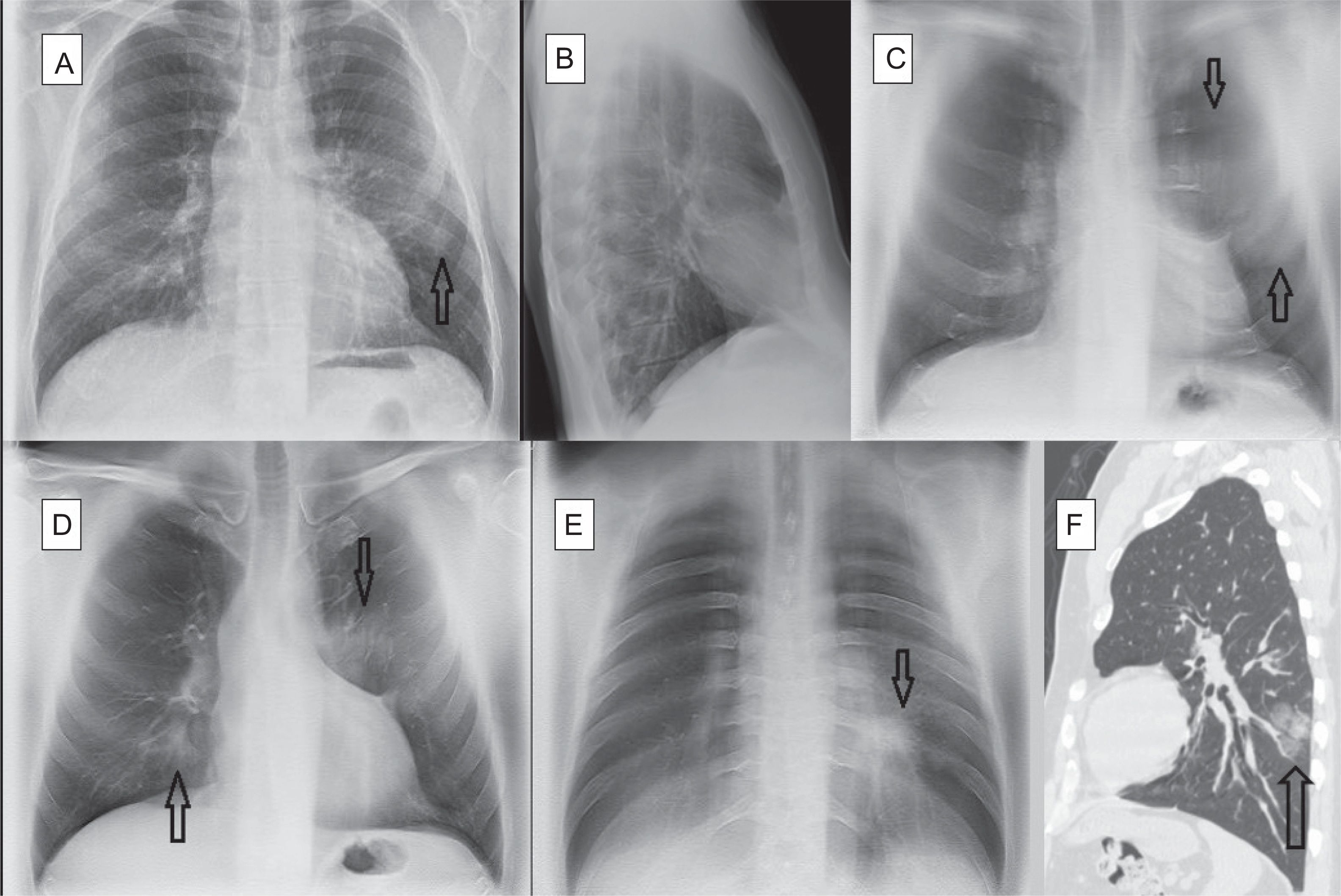
Our recent experience reporting DTS in patients with suspected COVID-19 suggests that this technique is more useful when pulmonary opacities are subtle and therefore more difficult to identify by X-ray. It also facilitates the detection of multiple peripheral opacities, confirming bilateral involvement in many cases; characteristics that, as already mentioned, are associated with COVID-19. In this respect, DTS is more specific than chest X-ray in this disease. By providing a series of coronal slices, pulmonary opacities that may be faint or posterior can be more accurately located than with lateral X-ray (Fig. 1) (annex, Supplementary Figs. 1 and 2). It is not a matter of opinion. It is a conclusion generated by what was experienced with these patients. The main limitation of this technique is the respiration-mediated artifacts caused by the difficulty of some patients in holding their breath during the examination.
Bilateral COVID-19 pneumonia. A 52-year-old man, family doctor by profession, presented with a 10-day history of cough and myalgia. Dyspnea and fever on examination. Laboratory tests: normal white cell count, ferritin 545.7 ng/mL (>322), and erythrocyte sedimentation rate 53 m/n (0–20). PCR positive for SARS-CoV-2. A— Posterior-anterior chest X-ray: slight opacity in the periphery of the left hemitorax, middle field. B—Lateral chest X-ray with no obvious findings. C—DTS: Image no. 8 (anterior). Extensive opacity in anterior region of left hemitorax (arrows). D—DTS: Image no. 14 (central). Bilateral pulmonary opacities, in the left suprahilar region (arrow) and right lower lobe (arrow). E—DTS: Image no. 36 (posterior). Oval opacity in retro-cardiac region (arrow). F—Non-contrast chest CT scan, sagittal reconstruction. Oval opacity in the periphery of the left lower lobe (arrow).
Although more studies are needed to consolidate the utility of DTS in a scenario with high clinical suspicion for COVID-19, it seems reasonable that a DTS positive for disease could obviate the need for CT. In this context, DTS use as primary imaging technique not only relieves the pressure on CT rooms, but also reduces the radiation dose delivered to patients. In conclusion, our preliminary results suggest that DTS may play an important role in the initial evaluation of patients with suspected COVID-19.
Please cite this article as: Calvo I, SantaCruz-Calvo S, Aranzana MG, Mármol P, Luque JÁ, Ramos F, et al. Tomografía Digital y COVID-19: un avance en la valoración de opacidades pulmonares. Arch Bronconeumol. 2020;56:761–763.