Thanks to their ecological plasticity, humans can live anywhere on the planet inhabited by any other animal species.1 In Peru, a country of 32 million inhabitants, approximately 32% of the population live in regions higher than 2500m above sea level (masl). However, Peru lies between parallels 0°2′ and 18°21′34″ of the southern hemisphere, and its proximity to the equator means that the weather is not excessively cold, so humans and other animal and plant species can survive at these heights in conditions of hypobaric hypoxia. According to popular belief in Peru, asthmatics should move to high altitudes because, they say, there is no asthma there. This is because the type of mites found change and their numbers decrease as we ascend, to the extent that they do not exist above 3800masl.2
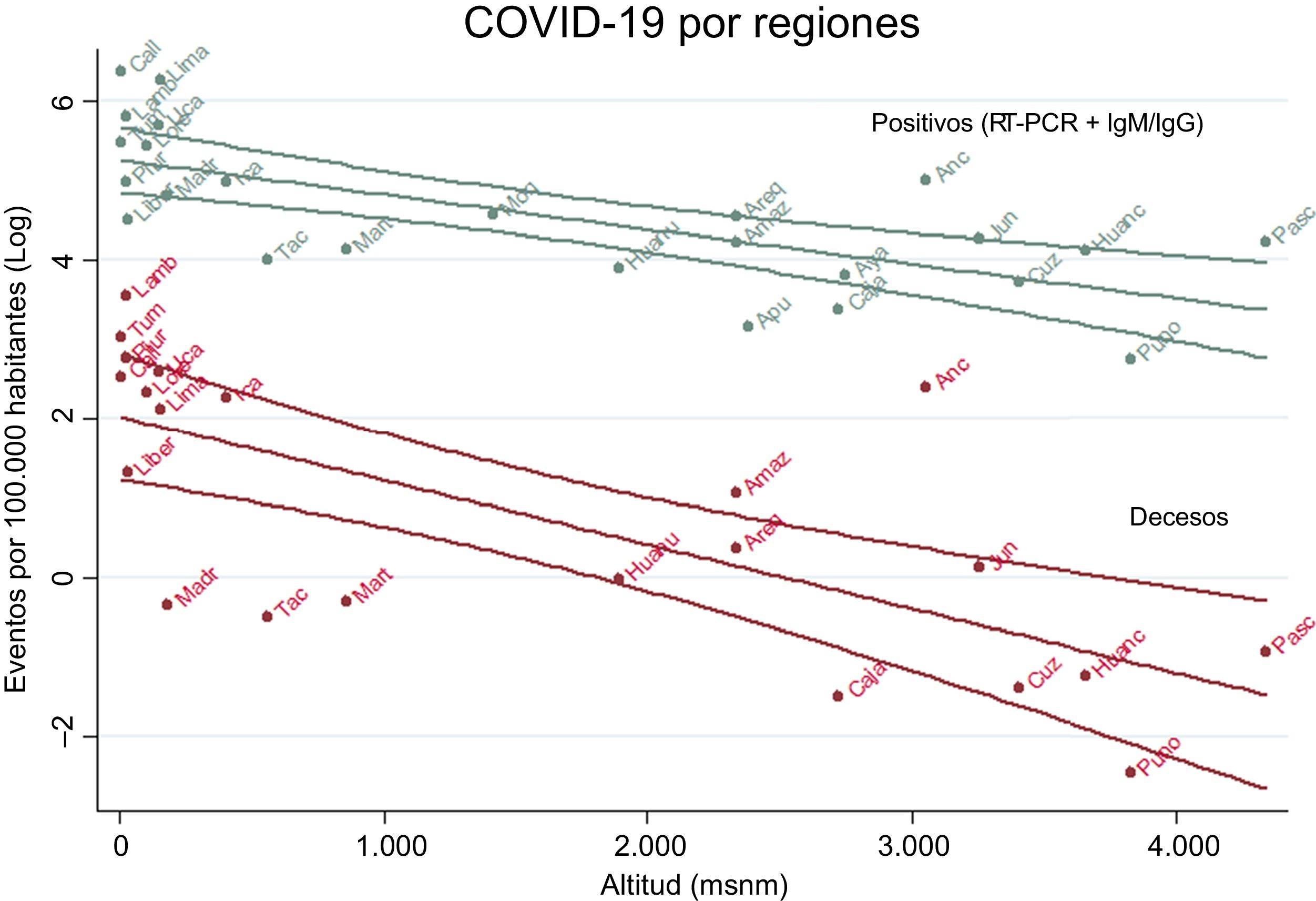
The first case of Peruvian COVID-19 was announced on March 7, 2020 and on March 15 the country went into lockdown to curb the pandemic, with curfews still being imposed at the time of writing. Over 170039 cases of COVID-19 have been confirmed by RT-PCR and IgM/IgG antibodies. An analysis of national data showed that the number of cases and deaths per 100000 inhabitants decreased as the altitude of residence increased (Fig. 1). Adjusting for sex and region size, the data show that for every 500 m increment in altitude, the rate of cases is reduced by 22% and deaths by 40%. The ratio of cases and deaths in regions below and above 2500masl is 4.5 and 10.9, with 3450 versus 774 cases and 76 versus 7 deaths, respectively (P<.05). It is important to note that above 2600 masl, COVID-19 mortality is estimated at less than 1/100000 inhabitants (P<.0001). This fraction is similar to figures published in Bolivia and Ecuador, which reported 3 to 4-fold lower infection rates at high altitudes than in the lowlands.3
Between 2009 and 2015 in San Jerónimo, Cusco (3244masl), there were 83 cases of influenza per 1000 person-year, while in Lima, Madre de Dios and Tumbes, located at sea level, there were 107, 108 and 104, respectively, almost 30% fewer cases than at high altitudes.4 A lower viral load was observed in mice acclimatized in a hypobaric chamber at a height of 9100masl who were inoculated with influenza virus, than in their sea level controls (log ID50 4.87 vs 6.97; P<.01).5 In animals inoculated at a simulated height of 6100masl, survival was longer in those who remained at that level after inoculation than in those that were returned to sea-level pressures.6 The lower frequency of COVID-19 at high altitudes cannot be attributed to hypobaric hypoxia alone, since in Peru the incidence of patients with influenza virus is only 30% lower at high altitude,4 whereas the rate of SARS-CoV-2 infection is 350% lower.
To penetrate cells, the S protein of SARS-CoV-2, pre-primed by serine protease TMPRSS2, binds to ACE2.7 SARS-CoV-2 preferentially infects well-differentiated ciliated epithelial cells that express ACE2, but not defective cells. In human pulmonary artery smooth muscle cells, overexpression of hypoxia-inducible transcription factor 1 (HIF1) upregulates the expression of the ACE protein and decreases the expression of ACE2. So in hypoxia, HIF1 production is increased, and ACE increases and stimulates the expression of angiotensin II (AT2) which regulates the AT1 receptors, reducing ACE2 expression.8 Fewer ACE2 receptors would explain the lower incidence of COVID-19 in high-altitude populations, and also the lower mortality rate, because if fewer ACE2 receptors are circulating, the viral load received by infected subjects, an essential factor in the course of the disease, will be lower.9 Hypobaric hypoxia increases erythropoietin (EPO), a multifunctional cytoprotective hormone, which decreases inflammation caused by septic shock and mitigates endotoxemic microvascular damage,10 factors which could also explain the lower COVID-19 mortality among patients living at high altitudes. In France, poor clinical and virological outcomes in COVID-19 patients treated with hydroxychloroquine-azithromycin were associated with the use of AT1 blockers.11 COVID-19-related mortality among men could be higher because ACE2 receptor expression is lower among women.12
One of the limitations of this study is that individual data were not used for analysis because they were not freely accessible. More complex research including variables such as age, symptoms, severity, and time-space patterns of infection is needed to determine whether COVID-19 severity varies with altitude.
Although this paper has the limitation that individual data were not used for the analysis because they were not freely accessible, we believe that the pathophysiological mechanisms we describe could explain why in Pasco, the region with the highest capital in Peru (4338masl), the COVID-19 infection rate is 174/100000, while in Callao, the lowest capital (7masl) in the country, it is 1106 (6.4 times higher). We agree with Soliz and Zubieta3 who previously proposed that the lower expression of ACE2 receptors was associated with the reduction of COVID-19 cases among high-altitude residents.
Please cite this article as: Accinelli RA, Leon-Abarca JA. En la altura la COVID-19 es menos frecuente: la experiencia del Perú. Arch Bronconeumol. 2020;56:760–761.