Persulfate salts are the agents most commonly associated with occupational asthma (OA) among hairdressers.1 Although the first cases were described decades ago, the prevalence, mechanism, value of diagnostic tests and the progress of these patients remain poorly defined. We present the case of a hairdresser with respiratory symptoms associated with exposure to persulfate salts in whom a specific bronchial challenge (use or exposure test) performed in the workplace was useful for confirming the diagnosis of OA.
A 30-year-old woman who began working as hairdresser at the age of 20. Rhinitis and bronchial asthma in childhood, subsequently asymptomatic. She presented with asthma, onset one year previously and poor control despite treatment. She had had several exacerbations while at work, requiring hospital care, for which reason she was referred to the Respiratory Medicine department.
Initial physical examination was normal. Of note on biochemistry was IgE 456IU/ml. Specific IgE (RAST/CAP method) was positive for Dermatophagoides farinae, Dermatophagoides pteronyssinus, Felis domesticus, Canis familiaris and Olea europea. Paranasal sinus and chest X-rays showed no pathological findings. Spirometry results were normal with FVC 3250ml (94%), FEV1 2670ml (97%) and FEV1/FVC 82, and post-bronchodilator test was negative. A non-specific bronchial challenge test was performed with increasing methacholine concentrations. FEV1 fell by 30% with a 1.56mg/l dilution, corresponding to a PC20 of 1mg/ml. Diurnal variability in peak expiratory flow (PEF) over one month was greater than 20%.
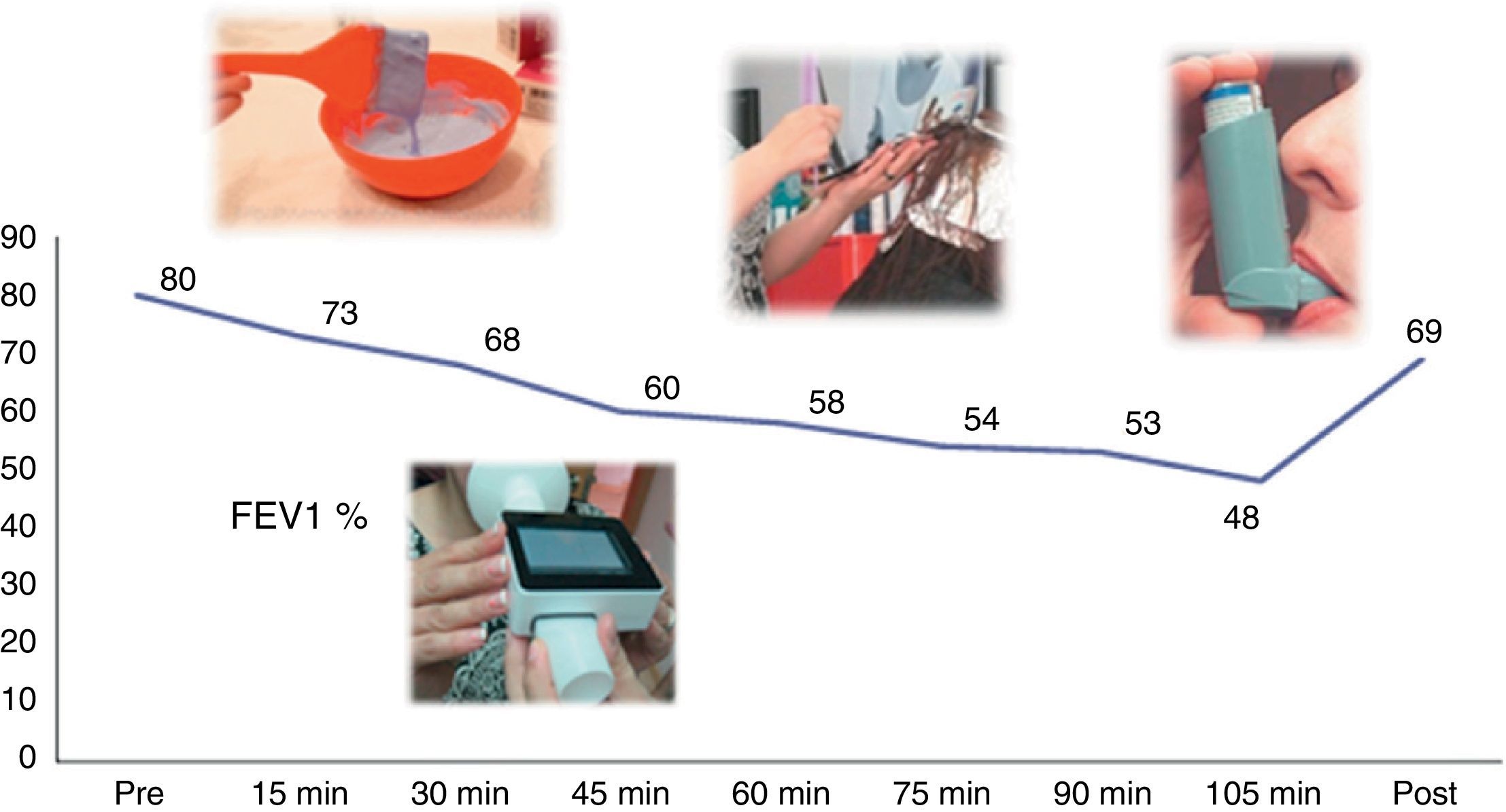
Correct treatment compliance adapted to her level of severity was confirmed, but the patient continued to show symptoms at work. She was asked again about the products she used and she indicated that it was the decolorizing agents that triggered the crises. The patient was asked to bring some along to the clinic and they were determined to contain persulfate salts. In view of suspected OA caused by persulfate salts, an “exposure test” was performed, consisting of monitoring lung function in her workplace using a portable spirometer. After baseline spirometry was shown to be normal, the patient began to use the bleaching agent as usual, lightening a client's hair (washing, decolorizing), while carrying out spirometries every 15min throughout the process. A fall in FEV1 >20% was observed, confirming the suspected diagnosis of OA due to persulfate salts (Fig. 1).
OA is the most common job-related respiratory disease in developed countries.2 One of the causative agents is persulfate salts, low molecular weight compounds that act as oxidants, accelerating the bleaching of hair with hydrogen peroxide. Hairdressers are the most exposed professional group.1 The mechanism appears to be immunologic, probably IgE-mediated, and there is a latent period between onset of exposure and the appearance of symptoms.1 With regard to diagnosis, specific bronchial challenge in the laboratory is considered the gold standard. When this is not available, specific bronchial challenge in the workplace is very useful.2–4 These patients progress well if exposure is avoided.2,5 However, 70% of them may continue to present symptoms and require treatment, even in the absence of exposure.
Please cite this article as: Pérez-Ferrer P, Landete P, Chiner E. Provocación bronquial específica en el trabajo y asma ocupacional por sales de persulfato. Arch Bronconeumol. 2014;50:497–498.