We report the case of a 47-year-old patient with iodinated contrast allergy and hypertension, diagnosed 2 years previously with low-grade malignant endometrial stromal sarcoma (ESS) treated with hysterectomy, double adnexectomy and bilateral pelvic lymphadenectomy. One year later she presented left retrosupravesical tumor recurrence that could only be partially resected, and received neoadjuvant radiation therapy and hormone therapy in the form of tamoxifen.
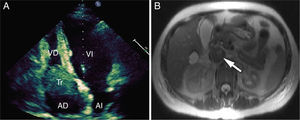
The patient presented with a one-week history of dyspnea on minimal effort. No significant findings were seen on chest X-ray. Significantly, a rapid ELISA test showed D-dimer of 1.141ng/ml, so lung scintigraphy was performed that confirmed bilateral pulmonary thromboembolism. Furthermore, a large mass in the right atrium that prolapsed into the ventricle during diastole with extension into the inferior vena cava (IVC) was observed on transthoracic echocardiogram (Fig. 1A). Magnetic resonance imaging (MRI) of the chest and abdomen (Fig. 1B) confirmed thrombosis occupying almost the entire lumen of the common iliac veins and the IVC, extending up to the right atrium. Gadolinium uptake was observed on inferior vena cava imaging, supporting the diagnosis of tumor thrombosis.
(A) Transthoracic four-chamber ultrasound, apical view, showing large thrombus in the right atrium shifting toward the right ventricle during diastole. AD, right atrium; AI, left atrium; Tr, thrombus; VD, right ventricle; VI, left ventricle. (B) Abdominal magnetic resonance image of inferior vena cava thrombosis.
Surgical intervention was ruled out in view of the partial resection of the pelvic tumor performed one year previously at the time of disease recurrence and because of her concomitant pulmonary thromboembolism. Enoxaparin 60mg every 12h and chronic oral anticoagulation were administered. Subsequent clinical progress was favorable, and after 30 months of follow-up the patient remains asymptomatic with an excellent performance status. Resolution of the thrombus in the right atrium and almost complete recovery of IVC patency have been observed on follow-up ultrasound and MRI.
ESS is a rare malignancy that accounts for only 0.2% of cancerous uterine tumors. The 5-year survival rate is 80%–100%. However, 30%–50% of patients present disease recurrence, generally after a long period of latency.1 Metastases most commonly occur in the vagina, the pelvis and in the peritoneal cavity. IVC tumor thrombosis and intracardiac tumor metastasis are extremely rare.2,3 Thus, although the prognosis of these tumors is good, they can appear to behave in a more aggressive manner.
Inferior vena cava tumor thrombosis is relatively common in renal carcinoma, and in these cases MRI is usually performed to confirm anatomical continuity between the tumor and the renal vein and the vena cava. Treatment of choice is surgery, and outcome in the absence of intervention is poor. In the case reported here, it was difficult to confirm anatomical continuity since the patient had undergone hysterectomy and double adnexectomy 2 years previously. The prognosis of endometrial stromal sarcoma is good, and its evolution and behavior cannot be compared to the considerably more aggressive renal cancer.
In the case of IVC and intracardiac thrombi, surgery is recommended for excision of the tumor thrombosis, with or without IVC resection, in order to prevent sudden death due to pulmonary embolism or the development of congestive heart failure or death due to acute valvular obstruction.4 We did not find any published cases of patients treated with anticoagulation only.
To conclude, it is safe to say that although surgery is the treatment of choice for IVC and/or intracardiac tumor thrombosis, for patients with advanced or inoperable disease or those who refuse surgery, chronic anticoagulation may also be a valid treatment option. In our view, there are probably many cases in which tumor thrombosis coexists with non-tumor thrombosis: it is easy to imagine that a lumen occupied by a tumor will favor the development of non-tumor thrombosis. This would explain the almost complete resolution of our case with anticoagulant treatment.
Please cite this article as: Garcipérez de Vargas FJ, Marcos G, Moyano Calvente SL. Embolismo pulmonar como primera manifestación de extensión intracardiaca de un sarcoma del estroma endometrial. 2014;50:498–499.