Primary esophageal achalasia, although rare, is a disorder of esophageal motility that is the result of a loss of ganglion cells responsible for motility and relaxation of the lower esophageal sphincter. As a result, patients present with worsening dysphagia to both liquids and solids and suffer from significant regurgitation of retained food, with weight loss and chronic cough. Achalasia symptoms may often mimic common diseases, and therefore, may delay the diagnosis.1
We report the case of a 10 years-old child who complained of barking cough from the age of 2 years and recurrent wheezing from the age of 3 years, with positive skin prick tests for alternaria. The child presented with frequent regurgitations in his first months of life, which subsequently disappeared.
Over the previous 6 months, the child had complained of epigastric discomfort and sensation of heaviness while eating, nocturnal cough and occasionally nocturnal emesis. Based on the change of symptoms, the family's pediatrician proposed treatment with long acting β2-adrenergic agonist (LABA)/ICS, without benefit. Admitted to a peripheral hospital, the child was transferred to our ward with the request to perform fiberoptic bronchoscopy and esophageal pHmetry for wheezing not responding to treatment and suspicion of gastroesophageal reflux disease. At admission he had body length of 141cm (25–50th percentile), body weight of 31.5kg (10th–25th percentile), transcutaneous oxygen saturation of 100%, respiratory rate 20 breaths per minute. Chest and abdomen examination were normal. Routine laboratory tests were normal, and allergy tests showed total IgE 193KU/L with specific IgE for alternaria 23.2KU/L. Spirometry revealed a flow/volume curve with reduction in PEF and FEV1 and a plateau consistent with tracheomalacia.
Fiberoptic bronchoscopy showed a tracheomalacia suggestive of aberrant innominate artery compression. The tracheal stenosis was fixed and pulsating, and the diameter remained constant with inspiration/expiration. The disease was localized where the vascular compression was present.
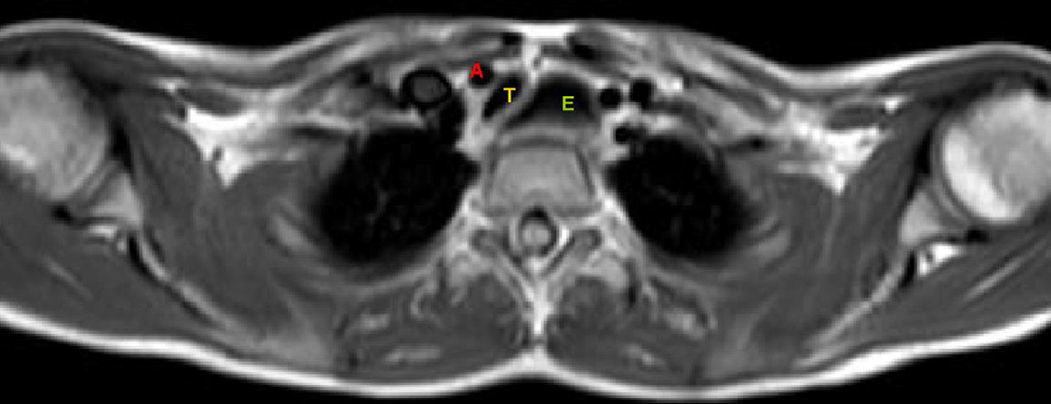
Spelunking the esophagus with the same instrument showed a severe dilatation. The child underwent esophagography, which showed a megaesophagus with “bird's beak appearance” of the distal portion, typical of achalasia; esophageal manometry confirmed the diagnosis. Magnetic resonance angiography of the thorax showed compression of the trachea against the innominate artery normally located, caused by megaesophagus (Fig. 1).
The patient underwent a laparoscopic Heller myotomy and Dor fundoplication with progressive resolution of symptoms.
The indication to perform the fiberoptic bronchoscopy in this patient was the recurrent wheezing not responding to treatment and chronic barking cough. The tracheomalacia shown during the procedure was first considered to be a consequence of aberrant innominate artery compression. Tracheomalacia can be caused by weakness of muscular wall and supporting cartilage due to external compression from abnormal vascular structures. In this patient, however, tracheomalacia was likely due to a displacement of the trachea caused by megaesophagus against the innominate artery normally located. The presence of burking cough from the age of 3 years shows that this tracheal anomaly was antecedent.
The incidence of achalasia in childhood is 0.11–0.18/100,000 children/year.2–4 The disease can manifest at any age, but onset of symptoms before adolescence is rare.3 Achalasia commonly manifests with dysphagia, post-prandial vomiting, failure to thrive and retrosternal chest pain or discomfort. Pulmonary symptoms may appear as a consequence of chronic inhalation of the esophageal stagnant content; children can present with chronic nocturnal wet cough, wheezing and recurrent pneumonia. Tracheal compression is also reported, due to bulging of megaesophagus against the trachea, together with cough, wheezing and/or stridor as prominent feeding or exercise correlated symptoms. Chest X-ray can be suggestive when presenting an air-fluid level in thoracic esophagus, a small/absent gastric air bubble and anterior displacement and bowing of trachea on the lateral view.2
Esophagography shows retained food in the esophagus and the “bird's beak “sign in the distal portion, suggestive of esophageal achalasia. Manometry will confirm the diagnosis. Pulmonary function tests can be useful, and fiberoptic bronchoscopy usually is not requested.
Heller's esophagocardiomyotomy is the treatment of choice for children with achalasia because of its safety and long-term effective results after surgery.5
In our patient, chronic barking cough was caused by a secondary tracheomalacia resulting from a shift of the trachea against the innominate artery normally located.
Please cite this article as: De Pieri C, Cogo P, Barbato A. Traqueomalacia debida a acalasia esofágica. Arch Bronconeumol. 2017;53:78–79.