Acute fibrinous and organizing pneumonia (AFOP) is a rare histologic interstitial pneumonia pattern described in 2002 by Beasley.1 It is usually idiopathic, but among the possible causes associated with AFOP, infections, autoimmune diseases, drugs, environmental or occupational exposures, cancers and organ transplantation have all been previously reported.2 We report the case of AFOP in a previously healthy woman.
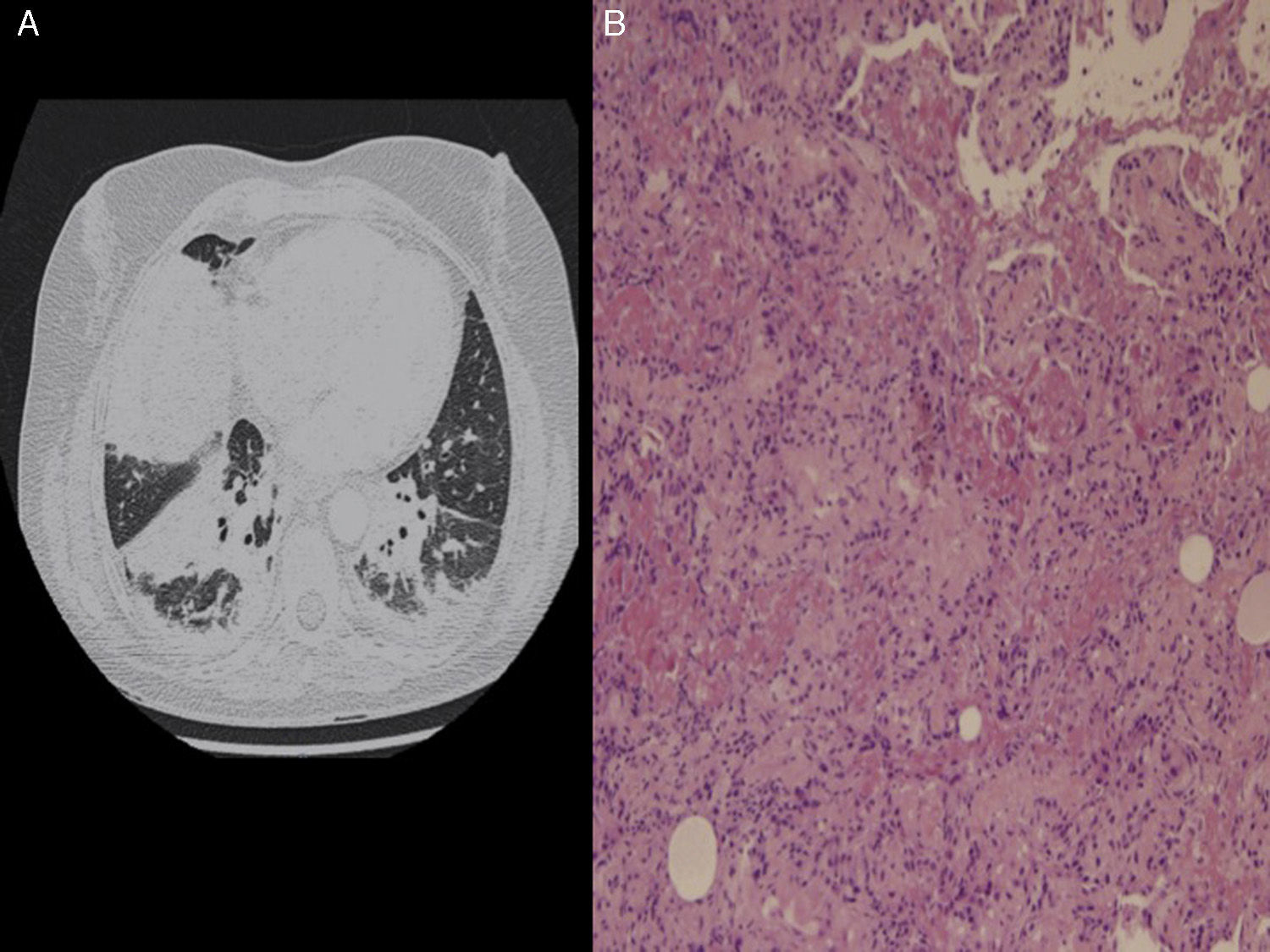
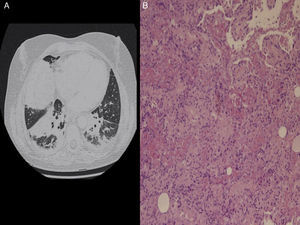
A 43-year-old woman presented to the emergency room (ER) with a 3-day history of worsening dyspnea along with intermittent fever since the previous week. She worked in a school as a teacher, and her personal history was unremarkable except for a smoking habit. She denied recent travels, environmental exposures and had no pets. Physical examination revealed bad general condition with fever, tachypnea, hypotension (95/69mmHg) and desaturation (oxygen saturation of 89% on room air). Moreover, inspiratory crackles in the base of the right lung were detected. Thorax X-ray demonstrated an alveolar opacification in the base of the right lung, and the main laboratory findings were a white blood cell count of 25,490leukocytes/mm3 and a C protein reactive of 40mg/dL. During her stay in the ER, quick clinical worsening was observed, with onset of severe respiratory failure and fluid-refractory hypotension, which led to the suspicious of a severe respiratory septic shock. The patient was transferred to the intensive care unit (ICU) for mechanical ventilation and empirical broad spectrum antibiotic therapy (meropenem 1g t.i.d and linezolid 600mg b.i.d). Nevertheless, thorax with contrast scan showed progression of the disease, with new dense bibasilar consolidations (Fig. 1A). Blood cultures, serology for atypical bacteria and bronchoalveolar lavage (BAL) with cultures for bacteria and PCR for respiratory viruses and mycobacteria were all negative. Transthoracic echocardiography ruled out heart dysfunction and antinuclear and antineutrophil cytoplasmic antibodies were negative. An open lung biopsy was performed and multiple intra-alveolar fibrin “balls” and inflammatory thickening of alveolar septa along with areas of organizing pneumonia with patchy distribution were observed, findings all consistent with the diagnosis of an acute fibrinous and organizing pneumonia (AFOP) (Fig. 1B). A 5 day treatment of methylprednisolone bolus (250mg q.o.d) was started, and progressive improvement in respiratory function was noted, thus allowing extubation and oral treatment with corticosteroids (60mg q.o.d for 2 weeks followed by gradual tapering). Eight weeks after ICU discharge, a complete resolution of respiratory symptoms and pulmonary infiltrates was achieved, so the patient was sent home with complete autonomy in her activities of daily living. Six months after hospital discharge, the patient remains asymptomatic on prednisone 7.5mg q.o.d, which is being progressively reduced.
Almost 120 cases of AFOP have been published in the medical literature, most of them idiopathic (as our case). It occurs most commonly in males in their fifth and sixth decade of life, and dyspnea is the most common symptom, sometimes accompanied by cough, haemoptysis or fever.2 Two clinical forms of the disease may be distinguished: a subacute variety with a gradual onset of the symptoms and mild or absent respiratory insufficiency, and an acute and rapidly progressing variety associated with fulminant respiratory failure and a very poor prognosis.3 The diagnosis of AFOP is challenging. Diffuse bilateral patchy infiltrates is the unspecific radiological pattern most commonly reported and BAL usually is inconclusive.2 Therefore, definitive diagnosis requires a lung biopsy, in which typical intra-alveolar fibrin “balls” and organizing pneumonia with a patchy distribution is observed.1 The differential diagnosis should always consider diffuse alveolar damage and eosinophilic pneumonia, marked by the presence of hyaline membranes and eosinophils, respectively.4 The recommended treatment for AFOP is high doses of methylprednisolone intravenously the first 3–5 days, followed by prednisone 0.5–1mg/kg per day, which is normally progressively tapered according to clinical evolution.2 Immunosuppressive drugs (mycophenolate mofetil, azathioprine and cyclophosphamide mainly) may be added to steroids from the beginning, but their utility seems to be higher in those cases of AFOP with often relapses and associated with autoimmune diseases.2
Our case illustrates that, given the rarity of AFOP and the requirement of a lung biopsy to reach the diagnosis, this entity may be underdiagnosed, and it is advisable to consider it in all those cases of pneumonia with an inappropriate response to anti-infective therapy.
Please cite this article as: Vargas-Hitos JA, Fernández-Muñoz J, Caba-Molina M, Jiménez-Alonso J. Una causa no habitual de distrés respiratorio del adulto. Arch Bronconeumol. 2017;53:79–80.