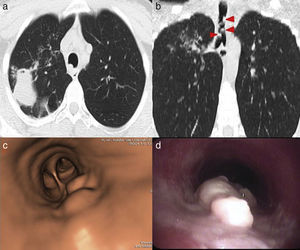
We report the case of a 28-year-old woman with Crohn's disease treated with adalimumab, azathioprine, and mesalazine. Mantoux and chest X-ray performed before treatment were negative. After 4 months of treatment, she presented with a 3-week history of cough, greenish expectoration, dysphonia, and cervical lymphadenopathy. Chest X-ray showed pulmonary consolidation with a cavitated area in the right upper lobe. On computed tomography (CT) (Fig. 1a), several nodular lesions were also observed on the posterior wall of the trachea (Figs. 1b and c), confirmed and biopsied by bronchoscopy (Fig. 1d). Ziehl-Neelsen staining of histological specimen revealed numerous acid-fast bacilli and growth of Mycobacterium tuberculosis was observed on culture. The diagnosis was pulmonary tuberculosis with tracheobronchial dissemination.
(a) Chest CT: cavitated lesion in the right upper lobe, associated with peripheral “tree-in-bud” micronodular pattern. (b) Several nodular thickenings are observed in the airway (arrow heads). (c) Virtual bronchoscopy: nodular lesions in the trachea. (d) Bronchoscopy: whitish soft-looking lesions attached to the posterior wall of the trachea.
Delay in detecting tracheobronchial tuberculosis can cause tracheal stenosis, atelectasis, postobstructive pneumonia, hemoptysis, and dyspnea.1,2 It tends to affect the main and upper right bronchi.2 CT is useful for diagnosis, as endobronchial lesions and the degree of stenosis can be evaluated,1,2 whereas the appearance of mucosa on bronchoscopy helps to predict the development of stenosis.2 Antituberculosis therapy can be supplemented with steroids,1 while tracheal stenosis may require endoscopic dilation techniques, or surgery as a last option.1,2
Please cite this article as: Gil Guerra AB, Gómez San Martín S, López Pedreira MR. Tuberculosis traqueobronquial. Arch Bronconeumol. 2018;54:41.