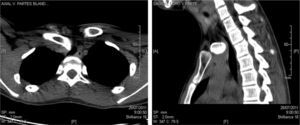
Posterior sternoclavicular dislocation (PSCD) is uncommon but may cause severe mediastinal injury. We report the case of a patient with PSCD and symptomatic tracheal compression requiring surgical intervention. This was a 16-year-old male with direct chest injury presenting with pain in the right shoulder and cough forty-eight hours after the event. On physical examination, deformity of the sternoclavicular joint and limited abduction (90°) was observed. The chest X-ray showed posterior sternoclavicular dislocation. Closed reduction was performed and the joint was immobilized with a sling. Fifteen days later, cough, stridor and breathing difficulties persisted. Computed tomography (CT) confirmed right PSCD with severe tracheal compression (Fig. 1). Surgery consisted of reduction and stabilization with cerclage wiring. The respiratory symptoms resolved.
Dislocation of the sternoclavicular joint is rare (<1%) due to the strength of the ligaments. It occurs in young people under the age of 25, the most common cause being traffic accidents (40%). A total of 95% are anterior, since the posterior ligaments are thicker and stronger than the anterior ones.1 PSCD is caused by anterior trauma to the clavicle (direct mechanism) or posterolateral trauma to the shoulder (indirect mechanism).2 Up to 30% of PSCD affect mediastinal structures such as the brachial plexus, brachiocephalic vein, innominate artery, trachea, bronchi and esophagus.3 Diagnosis is based on history, physical examination and radiology.4 Physical examination reveals loss of joint congruency, sternoclavicular depression, pain and functional impotence. Other symptoms are derived from the affected mediastinal structures: venous congestion, dysphagia, cough, dyspnea and stridor.1 Chest X-ray should be the initial examination undertaken (dislocation, costoclavicular fracture, pneumothorax, pneumomediastinum).4 Echography has been shown to be useful, but is not commonly used. CT is the test of choice for confirming PSCD and for excluding mediastinal complications.1–4 Magnetic resonance imaging can be performed in patients who are allergic to contrast media. Fiberoptic bronchoscopy is not essential for diagnosis. Treatment varies depending on the time since the event and associated injuries. Orthopedic intervention, consisting of closed reduction, is applied in PSCD within 48h of the event in the absence of mediastinal complications. However, this procedure fails in up to 50% of cases, with recurrence or unstable anterior subluxation.1 Surgical treatment consists of reduction and stabilization, and is indicated if more than 48h have elapsed after the injury, if closed reduction fails, if the joint is unstable, or if there is recurrence of the PSCD and mediastinal injury. Numerous stabilization techniques have been described, including fixation with nails or wire, joint reconstruction with subclavian tendon, sternocleidomastoid muscle and fascia lata (tenodesis), costoclavicular-clavicosternal cerclage and resection of the medial third of the clavicle.5 Late diagnosis and lack of treatment are often associated with complications such as arthritis, tracheoesophageal fistula or thoracic outlet syndrome.1,2 PSCD involving injury of the trachea is very uncommon. It should be suspected in patients with clavicle or shoulder injury who present respiratory symptoms. Diagnosis is based on CT and the treatment of choice is surgical reduction and stabilization.
Please cite this article as: Rodríguez Suárez PM, Hussein Serhal M, Freixinet Gilart JL. Compresión traqueal secundaria a una luxación esternoclavicular posterior. Arch Bronconeumol. 2014;50:306–307.