To evaluate the effect of a preparation with bacterial ribosomes and proteoglycans from Klebsiella pneumoniae “R” on the in vitro expression of CD11c and CD103 molecules in neutrophils from peripheral blood.
MethodsIsolation of neutrophils from peripheral blood with Ficoll-Paque, incubation with R and detection of CD11c and CD103 through flow cytometry.
ResultsSix hours after the incubation period, CD11c expression increased significantly as compared with the control with 125 and 500μg/ml of R (P=.017 and P=.006, respectively). CD103 expression induced with 125μg/ml of R after 6h was significantly higher than that observed after 4h at the same concentration (P=.014) and that found with 62.5μg/ml (P=.017) of R.
ConclusionsThe increased expression of CD11c and CD103 induced by R in the neutrophils could contribute to the R mechanism against respiratory pathogens.
Evaluar el efecto de una preparación con ribosomas bacterianos y proteoglicanos de Klebsiella pneumoniae «R» sobre la expresión in vitro de las moléculas CD11c y CD103 en neutrófilos de sangre periférica.
MétodosAislamiento de neutrófilos de sangre periférica con Ficoll-Paque, incubación con R y detección de CD11c y CD103 mediante citometría de flujo.
ResultadosA las 6h postincubación, la expresión de CD11c aumentó de manera significativa respecto al control con 125 y 500μg/ml de R (p=0,017 y p=0,006, respectivamente). La expresión de CD103 inducida con 125μg/ml de R a las 6h fue significativamente mayor que la observada a las 4h a la misma concentración (p=0.014) y que la encontrada con 62,5μg/ml (p=0,017).
ConclusionesEl aumento en la expresión de CD11c y CD103 inducido por R en neutrófilos podría contribuir al mecanismo de acción de R contra patógenos respiratorios.
Acute airway infections are one of the most important health problems in developing countries, causing 2 million deaths among children under the age of 5 and representing a very significant economic cost for regional health-care systems.1 This has led to the implementation of strategies for managing these infections in which the World Health Organization has emphasized the negative effects of the indiscriminate use of antibiotics.2 An alternative to the use of antibiotics is immunotherapy with the ribosomal fractions of Klebsiella pneumoniae, Streptococcus pneumoniae, Streptococcus pyogenes, Haemophilus influenzae and the proteoglycans of K. pneumoniae contained in Ribovac® (a formula of bacterial ribosomes and proteoglycans of K. pneumoniae), which is also marketed as Ribomunyl® and Immucytal®. It has been demonstrated to be effective for decreasing the recurrence and the duration of respiratory tract infections and the need for antibiotics for their control.3
One of the effects that R exerts in the immune system is the increased adhesiveness of peripheral blood neutrophils,4 which has been associated with the overexpression of the subunit β2 (CD18) of the CD11(α)/CD18 family of integrin heterodimers,5 which also participate in leukocyte rolling and diapedesis.6 The specific function of each member of this family of proteins depends on the type of α subunit to which CD18 is associated. Due to possible pleiotropic effects attributable to the wide variety of ligands for the different members of CD11, it is necessary to determine the impact of R on CD11c, which is very important in the leukocyte adhesion process.
Another adhesion molecule that is crucial for the innate responses of the respiratory tract mucosa is the integrin αE (CD103)/β7. It is involved in the adhesion and the transmigration of leucocytes among the epithelial cells in order to enable the capture of antigens in the airway lumen and the later presentation to virgin T cells in the bronchial lymph nodes.7
The objective of this study was to evaluate the effect of R on the expression of CD11c and CD103 molecules in peripheral blood neutrophils.
Materials and MethodsObtaining NeutrophilsThe separation of the neutrophils was done from the peripheral blood of healthy never-smoker donors using separation with Ficoll-Paque (δ=1.113) (Amersham Biosciences, Piscataway, NJ, USA), following the manufacturer's instructions. The cell viability was determined before each experiment by the trypan blue exclusion criteria. Cell viability was accepted at ≥95%.
Treatment with a formula of bacterial ribosomes and proteoglycans of K. pneumoniae and detection of CD11c and CD103
The cells (2×105cells/100μl) were treated with volumes of 20μl of R at final concentrations of 0, 62.5, 125 and 500μg/ml, and they were incubated for 4 and 6h at 37°C in a humidified atmosphere of 5% CO2. These concentrations were chosen because they had induced maximum concentrations of IL-6 and IL-1 cytokines in previous assays done in our lab. The detection of the adhesion molecules was done with an EPICS XCL flow cytometer (Beckman Coulter, Brea, CA, USA) using anti-CD11c-PE and anti-CD103-FITC monoclonal antibodies (Beckman Coulter, Brea, CA, USA).
The concentration of R was chosen based on the fact that in our lab, as well as in other laboratories, there had been a greater induction reported of the production of cytokines by the mononucleated cells activated by R. The neutrophil culture time was limited to 4 and 6h because their mortality rate is usually greater with greater times, and we had proposed to work with a cell viability of higher than 95% for the cells that were placed in the cell cultures.
Statistical AnalysisThe results were expressed as means±SD from at least 3 independent experiments. The statistical significance between the means was compared using the Student's t-test with a 95% confidence interval and a P-value<.05. All the procedures were done with the SPSS statistical package, version 18.0 (SPSS Inc., Chicago, IL, USA).
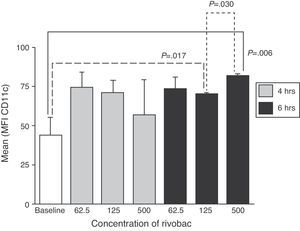
ResultsExpression of CD11cNo statistically significant changes were observed compared with the control in the expression of CD11c at all the concentrations of R with 4h of incubation (Fig. 1). After 6h, the expression of CD11c increased significantly as compared with the control with 125 and 500μg/ml of R (P=.017 and P=.006, respectively). Likewise, it was observed that the expression of CD11c induced with 500μg/ml of R was significantly greater than the expression of this marker in cells treated with 125μ/ml (P=.030).
Effects of the concentration of the formula with bacterial ribosomes and proteoglycans of K. pneumoniae and incubation time on the expression of CD11c in neutrophils. The results are expressed as mean±SD of the mean fluorescence intensity (MFI) of 3 independent experiments. The concentrations are expressed in μg/ml of R.
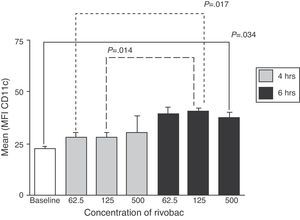
No statistically significant changes were observed as compared with the control in the expression of CD103 for all the concentrations of R after 4h of incubation (Fig. 2). After 6h, the expression of CD103 was greater than the control and at all the concentrations of R assayed but was only statistically significant with 500μg/ml (P=.034). However, the expression of CD103 induced with 125μg/ml of R after 6h was significantly greater than that observed after 4h at the same concentration (P=.014) and than that found with 62.5μg/ml (P=.017).
Effects of the concentration of the formula with bacterial ribosomes and proteoglycans of K. pneumoniae and incubation time on the expression of CD103 in neutrophils. The results are expressed as mean±SD of the mean fluorescence intensity (MFI) of 3 independent experiments. The concentrations are expressed in μg/ml of R.
Finding a sustained increase in the expression of CD11c and CD103 molecules in neutrophils treated with R during both 4 and 6h compared with cells that were not stimulated with R indicates that R induces a sustained effect up until at least 6h in vitro. This is important for explaining the capacity of neutrophils to mediate important cell adhesion events in order to activate cell populations involved in the response against respiratory infections. The maximum expression of CD11c as well as CD103 was reached 6h after the treatment of neutrophils with R, although at different concentrations of the preparation, which could be related with the different response of the receptors depending on the dosage and with the activation of different signaling pathways necessary for the expression of these molecules. The study of these conditions and of the participation of said molecules in innate immunity events against respiratory tract pathogens are recommendations for later studies.
One of the CD11c ligands is the ICAM-1 intracellular adhesion molecule,8 which participates in the firm adhesion to the endothelium and the leukocyte transmigration mediated by CD11b.9 Since CD11b and CD11c share the same functions,10 the overexpression of CD11c induced by R could implicate an increased capacity of the neutrophils to firmly adhere to the endothelium and transmigrate, which could be related with increases in the adhesiveness and the chemotactic migration associated with the overexpression of CD18 induced by R.4,5 The fraction of the iC3b is another of the ligands for CD11c11; therefore, the overexpression of CD11c could favor the phagocytosis mediated by this opsonin and contribute to the increase in the phagocytic capacity induced by R.12 On the other hand, an overexpression of CD11b has been detected (but not of CD11c) in the neutrophils of smoker patients with chronic obstructive pulmonary disease13; in contrast, an increase has been observed in the expression of CD11c in the neutrophils of patients with deep vein thrombosis.14 This reflects the importance of knowing the effects of R on the expression of the different members of CD11 for predicting potential adverse effects of R during respiratory inflammatory diseases and other unrelated disorders; in this regard, one of the limitations of this paper is that we did not study the effects of R on the expression of CD11a and CD11b.
As for CD103, the authors have not found reports of its expression in neutrophils, and this molecule has been detected in different subgroups of T cells and dendritic cells.7 The overexpression of CD103 induced by R can be important in their pharmacological mechanism of action due to the role that this molecule plays in leukocyte retention in the respiratory tract mucosa. This would imply that R could stimulate the local innate responses promoting the migration of neutrophils toward the area of inflammation during respiratory infections. Furthermore, it has been demonstrated that an increase in some leukocyte subpopulations that express CD103 can precede the development of respiratory allergic diseases.15 Therefore, more extensive studies are needed to corroborate the function of CD103 in neutrophils and their role in the immunity of the respiratory tract mucosa, which would enable us to evaluate whether the benefits of R surpass its potential negative effects in atopic patients or with inflammatory diseases. The overexpression of important adhesion molecules in neutrophils can be one of the mechanisms that explain the decrease in respiratory infections induced by R. This opens the possibility of studying on one hand the signaling pathways in which these molecules participate in order to analyze the magnitude of their contribution to the mechanism of action of R, while on the other hand investigating whether the overexpression of these molecules partially explain the rate of responsiveness to this biopreparation.
In conclusion, R stimulates the expression of CD11c and CD103 adhesion molecules in peripheral blood neutrophils. These effects suggest that the cytoadhesion mediated by these molecules induced by R boost the capacity of the neutrophils as effector cells that are active in the defense against respiratory tract pathogens.
FundingLaboratorio Pierre Fabre México has provided partial funding for this study through the RIBO-MEX-001-08 project.
Conflict of InterestsPartial funding was received from Laboratorios Pierre Fabre Mexico for this study.
Please cite this article as: Villa-Ambriz J, et al. Aumento de la expresión de las moléculas CD11c y CD103 en neutrófilos de sangre periférica tratados con una formulación de ribosomas bacterianos y proteoglicanos de Klebsiella pneumoniae. Arch Bronconeumol. 2012;48:316-9.