The risk of hepatitis B virus (HBV) transmission through donor organs with HBsAg(−) and anti-HBc(+) serology has not been extensively studied in lung transplantation. The objectives of this study are to ascertain the influence of the anti-HBc(+) on the acceptance of the lung for transplantation, to comment on the published literature and to suggest an algorithm for action.
MethodsA survey conducted in the 7 Spanish lung transplantation teams. The updated search of the literature was performed using medical databases from 1994 to February 2012.
ResultsAll of the teams vaccinate the lung recipients against HBV, although none quantify the anti-HBs titers. When given an anti-HBc(+) donor, 3 teams change their strategy: one does not accept the offer, one selects the receptor from among patients in emergency status and another adds pharmacological prophylaxis. Only 3 publications refer to the serologic evolution of the receptors. At the moment there have been no reported cases of hepatitis B or HBsAg positivity post-transplant, but 4 out of the 50 anti-HBc(−) receptors changed to anti-HBc(+) in the follow-up.
ConclusionsThe presence of anti-HBc in the donor influences the decision to accept a lung donor, although there is little information on its repercussions. To date, there has been no reported case of transmission of HBV, but post-transplant anti-HBc seroconversions have been described, which suggests contact with viral particles. Although rare, an anti-HBc(+) donor can harbor a hidden HBV infection. The risk of infection can be reduced with adequate anti-HBs titers or with appropriate pharmacological measures.
El riesgo de transmisión del virus de la hepatitis B (VHB) a través de órganos de donantes AgHBs(−), anti-HBc(+) está poco estudiado en el trasplante pulmonar. Los objetivos del estudio son conocer la influencia del anti-HBc(+) en la aceptación del pulmón para trasplante, hacer una puesta al día de los trabajos publicados y sugerir un algoritmo de actuación.
MétodosEncuesta dirigida a los 7 equipos españoles de trasplante pulmonar. La puesta al día se realizó mediante búsqueda en bases médicas desde 1994 hasta febrero del 2012.
ResultadosTodos los equipos vacunan a los receptores contra el VHB, aunque ninguno cuantifica los títulos anti-HBs. Ante un donante anti-HBc(+), 3 equipos modifican su estrategia: uno no acepta la oferta, uno selecciona el receptor a pacientes en situación de urgencia y otro emplea profilaxis farmacológica. Solo 3 publicaciones hacen referencia a la evolución serológica de los receptores. No hay descritos casos de hepatitis B, ni seroconversión del AgHBs, pero 4 de 50 receptores anti-HBc(−) positivizaron el anti-HBc en el seguimiento.
ConclusionesLa presencia del anti-HBc en el donante influye en la aceptación del pulmón para trasplante, aunque existe escasa información de su repercusión. Hasta el momento no se ha descrito ningún caso de transmisión del VHB. Sin embargo, se han descrito seroconversiones del anti-HBc, lo que sugiere contacto con partículas virales y, aunque poco frecuente, un donante anti-HBc(+) puede albergar una infección oculta por VHB. El riesgo de infección puede reducirse con títulos anti-HBs adecuados o con medidas farmacológicas.
The imbalance between the number of organ donors and the number of transplants needed causes the progressive increase in patients on waiting lists for lung transplantation.1 Approximately only 15% of organ donors in Spain are considered apt for lung donation.2 In some cases, preexisting lung damage, or that produced during brain death or while the donor is being maintained, prevent the organs from being used. In other cases, the risk of transplanting organs from older donors or donors with a history of neoplastic or infectious diseases causes them to be rejected.3–5 Likewise, potential lung donors with positive serology for hepatitis B virus (HBV) surface antigen, or HBsAg(+), are rejected due to the high risk of transmitting the disease to the recipient.6 However, there is some controversy about the potential transmission of the infection through organs from HBsAg(−) donors who are positive for the antibody against the core (anti-HBc). In these cases, there is a demonstrated high transmission through liver donation,7,8 but there is some debate, which is mainly derived from the lack of studies about the potentiality of infection through other organs. Some authors suggest that the risk for transmission through lung grafts would be more similar to liver grafts than heart and kidney transplants due to the greater content of lymphoid tissue and to the need for a greater degree of immunosuppression.9
A single positive result in the anti-HBc test can represent several levels of risk of transmission: high risk, due to an active infection with undetectable levels of HBsAg; undetermined risk in the lungs but high risk in the liver, as in cases of past infection that were cured with positive anti-HBc serology profile and positive or negative anti-HBs; or zero risk, due to the false positivity of the test.6,10 The risk also varies depending on the immunologic state of the recipient regarding B virus infection, be it due to previous contact or the vaccination itself.11
The importance of limiting cold ischemia time in lung transplantation usually impedes carrying out additional tests that could define this risk, meaning that occasionally transplant teams may rule out potentially useful organs. The consensus document “Selection criteria for organs donors regarding the transmission of infections”, created in 2004 by the National Transplant Organization and the transplant infections workgroup (GESITRA), concludes that when using the organs from a donor with this serology pattern, the recipients should preferentially be immunized patients or those with anti-HBs(+) or HBsAg(+), and they should always give informed consent.12
In recent years, between 8% and 10% of organ donors in Spain have been anti-HBc(+), which represents an important number of potential lung donors.2 Positivity is most frequent in older donors, who are currently the source with the highest growth rate for lung donor acceptance criteria.13
The objectives of this study are to know the influence of donor anti-HBc positivity on organ acceptance by different Spanish lung transplantation groups and to review the studies published in order to suggest a series of recommendations.
Material and MethodsIn order to analyze the influence of anti-HBc positivity on the acceptance of lung grafts for transplantation, in January 2011 we sent out an e-mail survey to the heads of the 7 Spanish lung transplantation groups. Said survey contained the following multiple-answer questionnaire:
- 1)
Do you routinely vaccinate against HBV in recipients on the waiting list?
- a.
Yes, during the routine recipient evaluation if their anti-HB markers are negative.
- b.
In addition to vaccinating, we periodically assess the state of protection.
- c.
We have never considered it.
- a.
- 2)
When donor organs are offered, do you specifically ask about anti-HBc?
- 3)
What are the steps of action when given an anti-HBc(+) donor? (More than one response may be selected.)
- a.
It does not influence in the decision to select the recipient.
- b.
The donor is rejected.
- c.
The organ is accepted only if the donor is also anti-HBs(+).
- d.
We select a recipient that is vaccinated against hepatitis B or has positive B virus markers.
- e.
It does not affect the decision, but we administer lamivudine and/or gamma globulin.
- f.
We use another strategy.
- a.
- 4)
When an anti-HBc(+) donor is accepted, is a specific consent model used?
- 5)
In the patients who have undergone transplantation in your Unit, have you detected cases of acute hepatitis B or seroconversions with uncertain origins?
- g.
No.
- h.
A few isolated cases.
- i.
More than 5 cases, at least.
- g.
- 6)
Add other comments that you consider to be important about the influence of anti-HBc in donors for organ acceptance or recipient selection.
The review of the literature entailed a search of articles from the Medline/PubMed database and EMBASE from 1994 until February 15, 2012 with the search terms “hepatitis B core” or “anti-HBc” or “occult hepatitis B” and “lung transplantation” or “transplant”, with no restrictions for the published language. The 2 authors reviewed the articles selected as well as their references in which a manual search was done to identify other potentially relevant articles or reviews.
ResultsAll the transplantation units answered the survey, and these responses are shown in Table 1. All seven groups regularly vaccinate against HBV in patients on the waiting list, although none quantify the level of anti-HBs titers. Six out of the 7 groups specifically request the donors’ anti-HBc. In the cases of positivity, one group does not accept this type of donors, another group selects the recipients from among vaccinated patients who are in relative emergency situations, and another group adds prophylaxis like lamivudine and/or specific immunoglobulin. Only 1 unit remembers having had occasional uncertain seroconversions. From among the comments solicited, 1 unit reported the importance of having more information about the serology of the donor, such as anti-HBc type, be it either Ig M or Ig G, anti-HBs marker and polymerase chain reaction (PCR) for hepatitis B virus.
Responses to the Survey.
| Unit | Vaccinate Recipients | Request Anti-HBc Information in the Donor | Accept Donors | Select the Recipients | Informed, Specific Consent | Prophylaxis | Cases of Post-transplant Seroconversion |
| 1 | Yes | Yes | Yes | No | Yes | Lamivudine and specific gamma globulins | No |
| 2 | Yes | Yes | Yes | No | No | No | No |
| 3 | Yes | Yes | Yes | No | No | No | No |
| 4 | Yes | No | Yes | No | Yes | No | No |
| 5 | Yes | Yes | Yes | Yes, in relative emergencies | Yes | No | Few isolated cases |
| 6 | Yes | Yes | Yes | No | Yes | No | No |
| 7 | Yes | Yes | No | No | No | No | No |
The order of the Units is according to the date when the completed surveys were received.
Anti-HBc, antibodies against the core.
In the bibliographic compilation, only 3 published studies10,14,15 were found that specifically referred to the serologic evolution of recipients of transplanted lungs from anti-HBc(+) organ donors, and they report the experience of 53 patients (Table 2). No recipients had developed hepatitis B or positive HBsAg, and 4 out of 50 pre-transplantation anti-HBc(−) recipients were later positive for this marker. Reference is made to the anti-HBs immunologic state in only 17 out of 50 receptors: 3 were positive for anti-HBc with pre-transplant anti-HBs titers <100IU/L and 1 with titers >100IU/L.
Studies Published on the Serological Evolution of Lung Recipients of Anti-HBc Donors (+).
| Author, Reference, Year, Country, Type of Study | No of Donors and Their Serology | No of Recipients and Their Pre-transplant Serology | Prophylactic Measures | Changes in Serology |
| Hartwig ME101992–2003USARetrospective | 29anti-HBc (+), anti-HBs(?) | 29Group 1: 26 anti-HBc(−), anti-HBs(?)Group 2: 3 anti-HBc(+), anti-HBs(?) | Pre-transplant vaccination (3 doses)No immunoglobulin or lamivudine | Group 1: No changesGroup 2: No changes |
| Fytili P141994–2004GermanyRetrospective | 17anti-HBc (+), anti-HBs(?) | 17Group 1: 11 anti-HBc(−), anti-HBs <100IU/lGroup 2: 6 anti-HBc(−), anti-HBs >100IU/l | No evidence of transmission of antibodies through transfusion | Group 1: 3 anti-HBc (+), HBsAg(−)Group 2: 1 anti-HBc(+), HBsAg(−) |
| Shitrit AB (15)1997–2005IsraelRetrospective | 7anti-HBc (+), anti-HBs(?) | 7anti-HBc(−), anti-HBs(?) | Lamivudine 100 mg/day, 1 year | No changes in the serologic profile |
The scarcity of organ donors causes changes in the classic donation criteria with regard to so-called “expanded criteria donors”.4,16 The demonstrated capacity for transmitting HBV infection through the liver of donors who present an HBsAg(−) serologic profile with anti-HBc(+) lead to these donors being considered as having expanded criteria. The acceptance of this type of donors varies between the different teams depending on multiple causes.17 This study shows that 6 out of the 7 lung transplant teams in Spain specifically request information about the anti-HBc serological state, and 3 of them clearly modify their procedure when given these donors. The remainder accept them, keeping in mind that the recipients are vaccinated for HBV, although none of them quantify the immunologic response after vaccination.
These decisions are probably based on reports published about other organ transplants because there are very few published studies about lung transplantation and, therefore, there are no guidelines or recommendations for this circumstance. In 2007, Dhillon et al. reviewed the UNOS (United Network for Organ Sharing) database in order to know the influence on mortality of lung and cardiopulmonary recipients who received the organs of anti-HBc(+) donors.18 After analyzing numerous factors in 333 patients transplanted with this type of donors and comparing them with 13,223 recipients of anti-HBc(−) donor organs, the authors concluded that there was no direct influence. This study, however, does not compile information about the transmission of the infection, nor of the pre- or post-transplant serologic or immunologic patterns of the recipients, or of the prophylaxis used.
Only 3 published studies retrospectively analyzed the serologic evolution of anti-HBc(+) donor lung transplant recipients. Hartwig et al.10 describe 29 patients in whom they found no seroconversion despite taking no prophylactic measures with either lamivudine or immunoglobulin. Although it does not offer any information about the anti-HBs immunologic state of the recipients, this study specifies that they were all vaccinated against hepatitis B. Fytili et al.14 described 17 patients and were the first to demonstrate post-transplant anti-HBc seroconversion in 4 of them (23.5%). These authors suggest that the anti-HBs titer prior to transplant is important for reducing the risk for transmission, as 27% (3 out of 11) of those with an anti-HBs level <100IU/L seroconverted, compared with 16% (1 of 6) of those who had an anti-HBs level >100IU/L. It should be noted that no patients turned positive for HBsAg or developed a clinical infection. Lastly, Shitrit et al.,15 suggest that the prophylactic administration of lamivudine in transplanted patients with lungs from anti-Hbc(+) donors may avoid seroconversion, although they do not offer information about the anti-Hbs state of the recipients prior to transplantation.
The number of lung donors is limited and, therefore, donors should not be ruled out without a justified reason. In recent years, up to 10% of organ donors had positive anti-HBc, representing an important number of potential donors. Anti-HBc positivity with HBsAg(−) can reflect several situations:
- •
Patients who have cleared HBsAg but have an acute infection in resolution or a chronic infection, or have a mutation of HBsAg that impedes its detection with standard techniques. In other words, they have a hidden infection for HBV and are potentially capable of transmitting it as has been demonstrated in transmission with blood transfusions of only anti-HBc(+) donors.19 In these cases, the serum determination of HBV DNA with PCR techniques could help outline the risk. The presence of HBV DNA in anti-HBc patients is variable depending on the population studied, being more than 35% in virus C or HIV carriers and between 0% and 7.4% in blood donors.20,21 As for transplants, Cirocco et al. reported an incidence of 0% in 53 organ donors,22 Challine et al. reported 3.1% (4 out of 129 organ and/or tissue donors)23 and Solves et al., in a Spanish study, found an incidence of 1.2% (1 out of 82 organ and/or tissue donors).24
- •
It may be a false positive, which is not uncommon enzyme-linked immunoabsorption assay (ELISA) techniques that are usually used for the detection of this marker. According to some authors, this may reach 20%-30% of determinations,6 but with the current use of more modern kits, this incidence is probably lower.
- •
It may represent a past, cured infection, in which case it is not usually accompanied by an anti-HBs marker. In these cases, the transmission of the disease through the liver is common, probably due to the hepatotropic nature of the virus,7,8,25 while it is uncommon through other organs,12 such as the heart26 or kidneys.27–29 However, the theoretical suggestion of some authors about the risk for transmission through the lung, more similar to hepatic than to cardiac or renal grafts due to the greater content of lymphoid tissue and the greater need of immunosuppression,9 could cause lung donations to be rejected.
On the other hand, transmission does not only depend on the serologic state of the donor and the transplanted organ but also on the anti-HBs immunity of the receptor and the prophylactic measures taken. For example, Madayag et al. recommend that patients on waiting lists for kidney transplants should not receive organs from anti-HBc(+) donors if they have anti-HBs titers <100IU/L.27 Two reviews published in 201030,31 suggest that the administration of oral lamivudine in recipients who receive livers from anti-HBc positive donors is as effective as the administration of immunoglobulin for maintaining anti-Hbs titers >100IU/L or as the combination of both strategies.
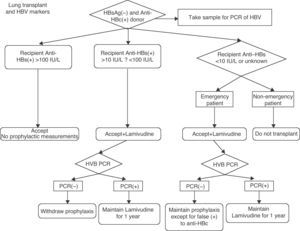
The importance of limiting cold ischemia time for lung transplants usually impedes carrying out additional tests that would allow for this risk to be defined at the time of the transplantation. The dilemma that arises is, therefore, what to do with these donors in the context of a progressively increasing waiting list and progressive decrease in the number of donors who are considered ideal for lung donation. Knowing that the risk is never going to be null and applying risk/benefit concepts, the following measures could be taken (Fig. 1):
- •
Routine vaccination against HBV for all patients on the waiting list and quantification of the anti-HBs response. The vaccination per se does not guarantee a proper immunologic response, even more so in patients with chronic diseases who are sometimes treated with glucocorticoids. Patients with titers >100IU/L could receive these organs. Patients with immunologic response >10IU/L and <100IU/L could receive the organs after prophylaxis. Patients with known anti-Hbs titers <10IU/L or unknown at the time the organ is offered should not receive these organs, unless in an emergency situation, and then only after taking prophylactic measures and with specific informed consent. In this situation, a sample should be taken in order to determine the anti-HBs immunity. The information received after the transplantation may aid in the decision to either continue or suspend the prophylaxis.
- •
Determination of donor viral PCR, with extraction of a sample by the lung transplant team and testing in the recipient hospital. As in the previous situation, the information received, probably deferred until after the transplantation, can aid in the decision to either continue with or suspend prophylactic measures.32 A negative PCR clearly reduces the risk and prophylaxis could be suspended in recipients with anti-HBs level between 10 and 100IU/L.
- •
It is not recommended to determine the type of Ig anti-HBc, whether it be IgM or IgG. Although it would discriminate the situation of acute infection in resolution from chronic infection, it is not a test that is done routinely and there are no published studies demonstrating that these practices should be changes depending on the type of Ig anti-HBc. Furthermore, the risk is better quantified with the result of PCR.
- •
The routine determination of donor anti-HBs is not recommended. Although a positive value in anti-HBc(+) donors would indicate a past and cured infection and not a false positive, its positivity does not rule out potential infection, as has been demonstrated in hepatic transplantations. High anti-HBs levels probably reduce or eliminate the risk for infection, but, as has been previously commented, the result of PCR offers more information. In addition, anti-HBs determination is also not a test that is done during emergency assessment of donor organs.
- •
In the previously described patients at risk, prophylactic administration of oral lamivudine or another specific antiviral medication is recommended,33 starting at the time of the transplantation itself. The use of immunoglobulin or the combination of immunoglobulin and lamivudine does not seem to provide greater benefits than the use of lamivudine alone.
It must be said that the recommendations are only theoretical and that controlled studies are needed to outline risk and demonstrate anti-HBs titers as well as the most effective pharmacological measures for prevention.
In summary, there is not much information in the literature about the evolution of lung recipients from anti-HBc(+) donors. To date, there are no descriptions in the literature of any cases of transmission of hepatitis B virus infection through the lungs from this type of donors. Nevertheless, anti-HBc seroconversions have been reported after transplantation, which suggests contact with viral particles and, in addition, there is the possibility that a donor with anti-HBc(+) could host a hidden B virus infection. The risk of infection may be lower with adequate anti-HBs titers either post-vaccination, post-infection or with pharmacological therapy.
Conflict of InterestThe authors declare no conflict of interest.
Please cite this article as: Chamorro C, Aparicio M. Influencia de la positividad del anti-HBc en el donante en la selección del donante pulmonar. Arch Bronconeumol. 2012;48:320-4.