Difficulties associated with disconnecting patients from mechanical ventilation and decannulation after prolonged ventilation are well documented. In most patients (70%), weaning is simple, but it is difficult in 15%, and prolonged in another 15%.1,2 In this last group, it is important to provide global, specialized management.
We report the case of a 50-year-old woman admitted to the intensive care unit (ICU) for 1.5 months after surgical resection of an occipital arteriovenous malformation. Because of the weaning difficulties experienced by this unit, the patient was transferred to an intermediate respiratory care unit (IRCU), where the following mechanical ventilation weaning and decannulation protocol was implemented3:
Phase 1. Assess the global situation
The patient had a prolonged stay in the ICU due to difficult-to-control focal epilepsy after surgery, which led to prolonged connection to invasive mechanical ventilation (IMV), with surgical tracheostomy performed at 2 weeks. Complications included IMV-related pneumonia4 and severe critical illness polyneuromyopathy.5 She required high positive end-expiratory pressures (PEEP) (20–25cmH2O) to maintain adequate alveolar recruitment. On arrival at the IRCU, she was totally ventilator-dependent, with pressure support (PS) ventilation (PEEP: 12, PS: 8, FiO2: 60%).
Phase 2. Assess the feasibility of spontaneous ventilation
The spontaneous ventilation test failed, due to a low respiratory drive, severe malacia that made it impossible to decrease PEEP due to collapse, a lack of cough effort, and severe diaphragmatic dysfunction, confirmed by chest ultrasound.6,7 Mucociliary clearance techniques began with respiratory physiotherapy, postural changes, active humidification systems aimed at reducing the viscosity of secretions, and regular aspiration of secretions 2–3 times every 8h, using a 12 CH suction tube.8,9
Phase 3. Choice of ventilation mode
As mentioned above, we decided to switch to pressure control mode until the respiratory drive improved, requiring a fixed inspiratory time (Ti), adjusted to the patient's neural Ti.10 With the aim of avoiding asynchronies (prolonged inspirations and double triggering), the sweep procedure was performed, consisting of increasing and/or decreasing the Ti of the ventilator until the one that is best suited to the patient was determined (Fig. 1A–C).
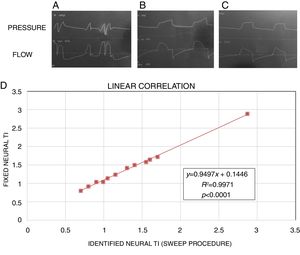
Sweep procedure to calculate neural inspiratory time (Ti). (A) Neural Ti greater than ventilator Ti, demonstrating double-trigger asynchrony. (B) Neural Ti less than ventilator Ti, demonstrating prolonged inspiration asynchrony. (C) Adjusted Ti with correct adjustment to ventilator. (D) Linear correlation between neural Ti and adjusted Ti obtained with the sweep method.
In addition to motor and respiratory physiotherapy, diaphragm muscle training sessions were conducted to address the problem of diaphragm dysfunction: the patient was connected for short periods of time to incremental pressure triggering, since this has been shown to increase the mechanical load more than flow triggering.11 After several sessions, diaphragmatic excursion improved, and respiratory drive and cough strength increased. Given the patient's clinical and mechanical progress, we decided to move forward and resume pressure support ventilation.
Phase 4. Assess tracheal integrity by performing a cuff leak test
A cuff leak test12 was performed, which was positive, with a difference in exhaled tidal volume of greater than 130ml.
Phases 4–7. Change of cannula and progressive closure
The cannula was initially substituted with a cannula with fenestra, which was closed for periods of 1–2h. High flow nasal prongs were used during closure periods, given their benefits in controlling malacia and decreasing airway resistance. In parallel with clinical improvement, the need to aspirate secretions diminished until an effective cough was achieved.
Phases 8–11. Placement of hemi-cannula, closure, and withdrawal
After checking tolerance to cannula closures for periods longer than 4–6h and confirming adaptation to and effectiveness of non-invasive mechanical ventilation (NIMV), we proceeded to place a hemi-cannula with cap, which was withdrawn 3–4 days later, with no complications. After successfully completing this protocol, the patient was transferred to the Department of Neurosurgery, where she continued to receive NIMV sessions without further incidents.
The sweep method used in this case is not described in the scientific literature, so a double-blind simulation of this procedure was performed. This was done using a lung simulator,13 in which a first operator sets a neural Ti and a second operator ventilates the simulator in pressure control mode and uses the sweep method to determine neural Ti. The procedure is repeated with different neural Ti values (n=12). Correlation using simple linear regression between the two Tis was R2=0.9, P<.0001 (Fig. 1D). In accordance with this result, we believe that this procedure can offer new possibilities in the neural control of ventilation in controlled modes.
It also raises the possibility of using high flow during closures with tracheotomy to manage tracheal malacia, given the advantages of this approach in the pressurization of the upper airway.14
We also describe a new modality of diaphragm training based on the use of pressure triggering, a method that has been abandoned in routine practice due to the greater work of breathing than observed with flow triggering. However, in our patient we took advantage of this effect to train the diaphragmatic muscle, monitor its activity by ultrasound, and control the risk of muscle fatigue (ineffective effort).
In conclusion, we highlight the relevance of the use of the sweep method in the neural control of ventilation and highlight the importance of having a highly specialized environment where a comprehensive protocol can be implemented for the management of patients with highly complex respiratory problems, such as prolonged weaning.
Please cite this article as: Herrero Huertas J, Laso del Hierro F, Peláez Castro F, Plaza Moreno C, Ampuero López A, Carballosa de Miguel MP, et al. Importancia del manejo especializado en el destete prolongado. Arch Bronconeumol. 2019;55:443–444.