Post-thoracotomy pain is a symptom of high incidence among patients who have undergone thoracotomy and is a major risk factor in the pathogenesis of several postoperative complications. Chronic pain after thoracotomy reaches a high prevalence. Since the earliest studies, this pain has been seen to be related with intercostal nerve injury, thus the need to avoid these lesions during thoracotomy has been recommended. This review aims to establish the appropriate surgical procedure for closure of the thoracotomy through a systematic review of the literature and analysis of levels of evidence provided by the studies found.
After an exhaustive search in MEDLINE, EMBASE, IME, IBECS and Cochrane Library, few studies were found. Each focuses on different aspects of thoracotomy surgical techniques, with a common denominator focused on the preservation of the intercostal nerves, and conclusions with different levels of evidence.
El dolor postoracotomía es un síntoma de alta incidencia entre los pacientes sometidos a toracotomía, que actúa como factor de riesgo importante en la patogénesis de diversas complicaciones postquirúrgicas. Su cronificación postoracotomía alcanza una alta prevalencia. Desde los primeros estudios se observó su relación con la lesión de los nervios intercostales y la conveniencia de evitar su lesión durante la toracotomía. Esta revisión pretende establecer el procedimiento quirúrgico más adecuado para el cierre de la toracotomía, mediante una revisión sistemática de la literatura médica y el análisis de los niveles de evidencia que proporcionan los estudios hallados.
Tras una búsqueda bibliográfica exhaustiva en MEDLINE, EMBASE, IME, IBECS y Biblioteca Cochrane Plus, se hallaron escasos estudios. Cada uno de ellos se orienta a distintos aspectos de técnica quirúrgica en toracotomía, con el denominador común del enfoque hacia la preservación de los nervios intercostales, y conclusiones con distintos niveles de evidencia.
Post-thoracotomy pain is a symptom with a high incidence among patients who have undergone thoracotomy. It is frequently an important risk factor in the pathogenesis of several post-surgical complications.
Pain is defined by the International Association for the Study of Pain as an “an unpleasant sensory and emotional experience associated with tissue damage”. Chronic post-thoracotomy pain (or post-thoracotomy neuralgia) is defined by the same Association as a “pain that recurs or persists along a thoracotomy scar for at least 2 months following the surgical procedure”.1
Its characteristics are those of neuropathic pain and, despite its incidence and clinical transcendence, its relationship with the affectation of the intercostal nerves has been the topic of very few studies in the medical literature. For some authors, it is the most common complication after thoracotomy. One study compiles several factors associated with its development: intercostal nerve injury, rib fracture, local infection, chondral affectation, tumor recurrence and psychological aspects.2
The first reference of chronic post-thoracotomy pain dates from 1944 and it was based on observations of US Army surgeons after treating chest trauma during World War II. After neurological exploration, they were able to conclude that the symptoms were related with the injury to the intercostal nerves; therefore, they recommended avoiding such injury during surgical procedures.3
Perttunen et al.4 carried out a follow-up study in 67 out of 110 initially recruited-patients. The study determined the levels of post-thoracotomy pain at 1 week, 3 months, 6 months and 12 months after an elective thoracotomy in patients treated with the same analgesic protocol. Out of the 67 patients followed up, 80% presented pain 3 months later, 75% 6 months later and 61% one year after the intervention. The pain was severe in 3%–5% of patients, and a correlation was found between a high consumption of analgesics during the first week post-op (evidencing immediate intense post-operatory pain) and the development of chronic pain.
Using the Cochrane Collaboration protocol, a group of anesthesiologists and surgeons, with the support of the European Society of Regional Anaesthesia and Pain Therapy, systematically reviewed the analgesic interventions aimed at a specific surgical procedure, presented under the name of Prospect (Procedure-Specific Postoperative Pain Management).5 There is growing evidence that the effectiveness of analgesic agents varies among different surgical procedures.
For the thoracotomy, the Prospect group did a systematic review of the literature from 1966 to May 2004 using MEDLINE and EMBASE and following the Cochrane Collaboration protocol. Randomized studies were included that evaluated analgesic interventions in thoracotomy and that registered the pain on a linear analogical scale. They identified 332 studies of perioperative interventions: 169 studies were included and 163 studies were excluded; the most common reason for which they were excluded was the lack of randomization (60 studies). This systematic review concludes with a series of recommendations that are evaluated according to the level of evidence that supports them, in accordance with the Oxford Centre for Evidence-based Medicine. These recommendations include pre-operative, peri-operative and post-operative analgesic interventions, as well as some aspects of surgical techniques. As for the choice of operative technique, this is generally determined by other factors other than post-operative pain (level of evidence: grade D). However, the recommendations do state that: whenever possible, anterior thoracotomy should be considered as it can reduce post-operative pain compared with posterolateral thoracotomy; thoracotomy using muscular separation reduces post-operative pain over the conventional technique; the use of intracostal sutures can reduce post-operative pain compared with the use of pericostal sutures; intercostal muscle flaps are also associated with less pain.
As for the approach method, there are several studies that do not find significant differences between posterolateral thoracotomy, thoracotomy with muscular separation and video-assisted thoracoscopic surgery in terms of developing post-thoracotomy chronic pain. Nevertheless, some randomized studies do establish such differences. In any case, it is not the approach techniques that are the subject of this review, but it is instead the techniques for handling the intercostal space. Rogers and Duffy2 conclude that post-thoracotomy pain is fundamentally due to damage to the intercostal nerve, more than the approach technique, and that efforts should be aimed at careful management of the intercostal space.
In conclusion, several studies have dealt with various aspects of surgical procedures and their relationship with post-thoracotomy pain, which is occasionally severe and even incapacitating. These studies have emphasized the importance of careful treatment of the intercostal nerves, while avoiding their injury. The best technique for meeting this objective with regards to the approach chosen, the incision technique and closure of the intercostal space, has been the center of these studies.
ObjectivesThe aim of this study is to be able to establish the most adequate surgical procedure for the approximation suture of the costal plane which minimizes the intensity of post-operative pain and prevents the development of chronic post-thoracotomy pain. To this end, we have systematically reviewed the literature.
Material and MethodsA bibliographic search was done in MEDLINE, EMBASE, IME, IBECS and the Cochrane Library Plus. The key words used were: “pain”, “thoracotomy” and “suture”, as well as their Spanish equivalents in the Spanish-speaking databases, with no truncation or annotation of any type.
The inclusion criteria were any type of study specifically centered on the relationship between surgical technique and post-operative pain. We have therefore excluded all the studies not directed at establishing the connection between the surgical technique used and the results of post-operative pain.
ResultsThe search done on MEDLINE through PubMed (http://www.ncbi.nlm.nih.gov/pubmed) obtained 63 results. After reviewing them, 8 were considered valid.
In EMBASE, the same search profile was used (http://www.embase.com/search/results), obtaining 111 references, from which 8 studies were selected.
The same search was done in IME (http://bddoc.csic.es:8080/inicioBuscarSimple.html?tabla=docu&bd=IME&estado_formulario=show), IBECS (http://ibecs.isciii.es/cgi-bin/wxislind.exe/iah/online/) and Cochrane Library Plus (http://www.bibliotecacochrane.com/), with negative results in all three.
Out of the articles found in MEDLINE and EMBASE, 7 articles were common to both. Thus, in the end 11 publications were obtained that met the search objective.
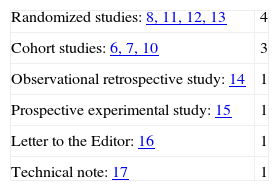
The references found were all journal articles: 4 randomized studies, 1 retrospective study, 1 letter to the editor, 1 experimental and prospective study (animal experimentation), 3 cohort studies and 1 technical note (Table 1).
After considering their content, the articles were grouped in the following manner, according to surgical aspects (always related to post-thoracotomy pain): 6 articles dealing with thoracotomy closure techniques (1 randomized study, 1 retrospective study, 1 letter to the editor, 1 prospective experimental study, 1 cohort study, 1 technical note); 3 articles about the closure of said space with resorbable osteosynthesis material (2 cohort studies with absorbable needles and 1 randomized study with resorbable plates); finally, 2 studies (both randomized) comparing a thoracotomy closure technique combined with an intercostal separation technique vs a thoracotomy closure method (Table 2).
Articles According to Topic (With Bibliographic References).
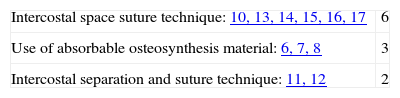
| Intercostal space suture technique: 10, 13, 14, 15, 16, 17 | 6 |
| Use of absorbable osteosynthesis material: 6, 7, 8 | 3 |
| Intercostal separation and suture technique: 11, 12 | 2 |
Despite the importance of basic surgical aspects in the pathogenesis of post-thoracotomy pain, there is very little related scientific evidence compared with an enormous number of papers that insist on pharmacological treatment and/or using local-regional anesthesia techniques. From a bibliometric standpoint, it is striking that we were not able to find one single study in the main Spanish bibliographic databases (IME, IBECS), nor were we able to find any reviews in the Cochrane Library Plus on the related evidence. Only one of the publications belongs to a work group in our country and is related to the use of osteosynthesis material.6
Upon analyzing the studies found, we verified that they are different types of studies about different aspects of surgical techniques. The articles are commented below in groups by topic.
The Use of Resorbable Osteosynthesis MaterialTwo papers were found that analyzed the use of absorbable osteosynthesis needles, and both were cohort studies. One analyzed the closure of the thoracotomy in patients who underwent thoracolaparotomy due to hepatectomy.7 It included 18 patients, 9 of whom were sutured without fixation of the rib edges, while in the remaining 9 resorbable osteosynthesis material was used. Pain was measured after one month, 2 months and 6 months, and the stability of the chest wall was checked. Significant differences were found in all the evaluated criteria which favored the use of osteosynthesis material. This study has a very relative value for the analysis that follows this study, as it comments on a very specific and unusual approach (thoracolaparotomy) that is different from conventional thoracotomy. Nevertheless, there are some very significant differences in favor of the use of this type of material in a procedure that causes intercostal damage, and which runs its course with intense post-operative pain as a frequent adverse effect.
The other study includes 33 consecutive patients with lung cancer who underwent lobectomy by means of posterolateral thoracotomy,8 and it analyzes immediate, acute, post-operative pain. Out of the total, 21 patients underwent an intercostal approach with absorbable osteosynthesis material, and the other 12 patients received conventional sutures. The pain was measured during the first 3 days post-op using an analogical-visual scale, and all the patients were treated with the same post-operative analgesic protocol. The resulting pain and the analgesic requirements were significantly less in the group who were treated with resorbable osteosynthesis material. As has been stated, this was a non-randomized study. Another important limitation of the study is the orientation of objectives towards short-term results: there was no later follow-up of the patients; therefore, the effect of this procedure on chronic post-thoracotomy pain is unknown.
A third study, the only in this review published by Spanish authors,6 analyzes the results of using resorbable osteosynthesis plates. It is a randomized, prospective study of patients who underwent thoracotomy with indication for lobectomy due to lung cancer, but it was published as a congress communication. It included 31 patients: in 15, the intercostal space was set with plates, and in 16 the classic intercostal suture (pericostal) was performed. Morbidity and mortality were assessed 2 months later. No statistically significant differences were found between the two groups, which the authors attribute to the lack of statistical power as it was a preliminary study. There was an observed more favorable tendency in the group in which absorbable plates were used for closure, and the morbidity was similar in the two groups; there was no mortality in the series.
Intercostal Suture Technique Combined With Intercostal Separation TechniqueTwo randomized studies with this focus have been found.
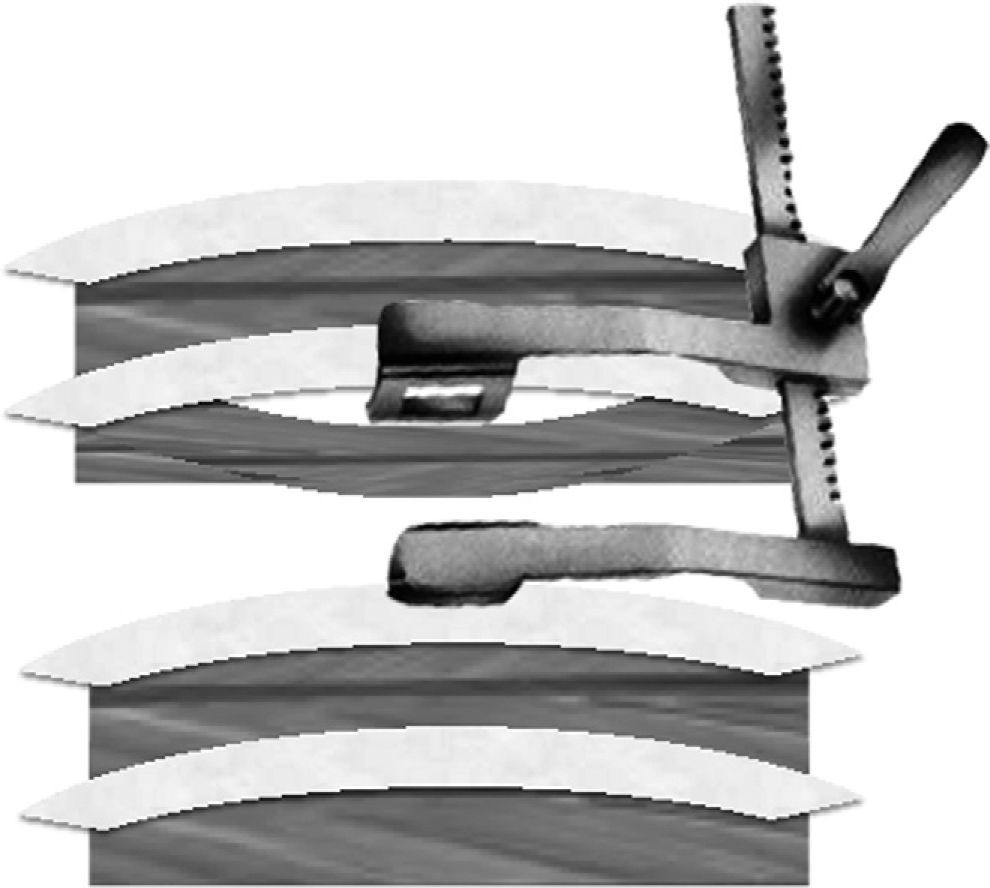
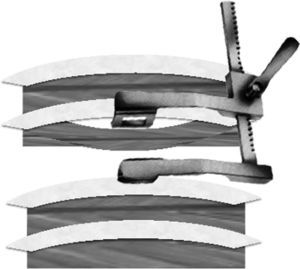
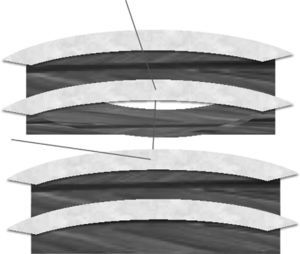
The intercostal separation technique entails moving the intercostal plane in the area where the spreader is supported (Fig. 1). This opening method, described by Cerfolio et al.9 in 2005, has been the subject of several randomized studies that have supported its effectiveness, although its use has not been generalized.
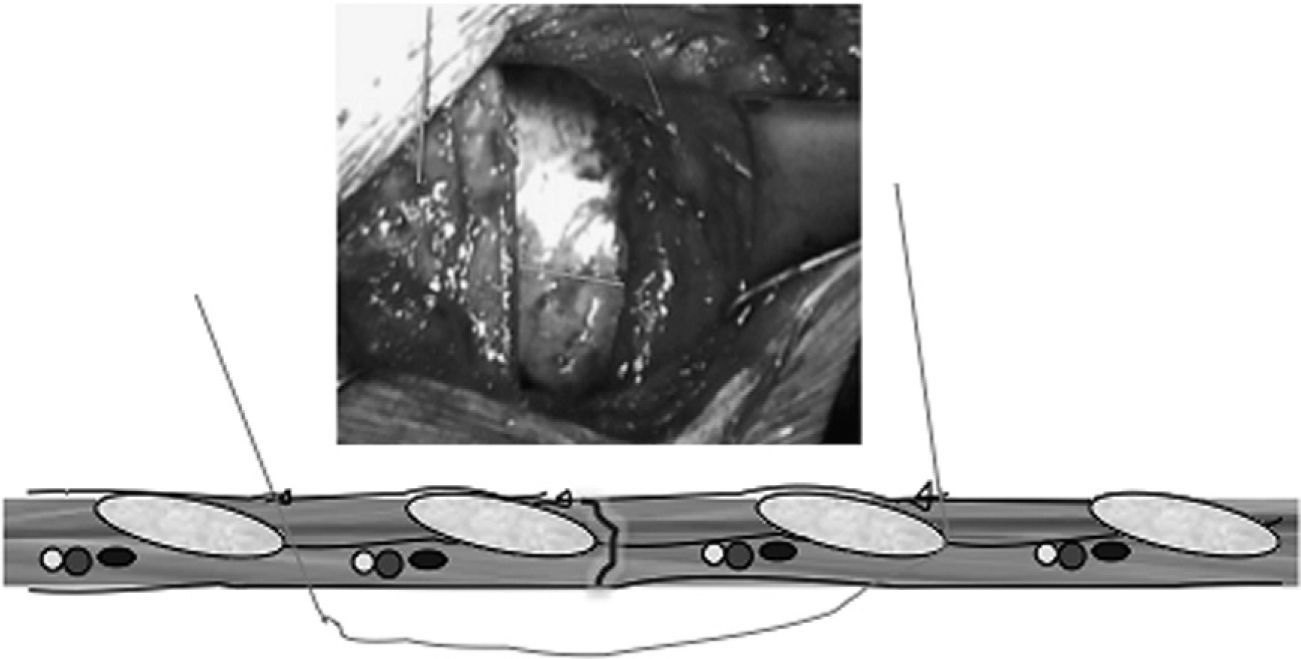
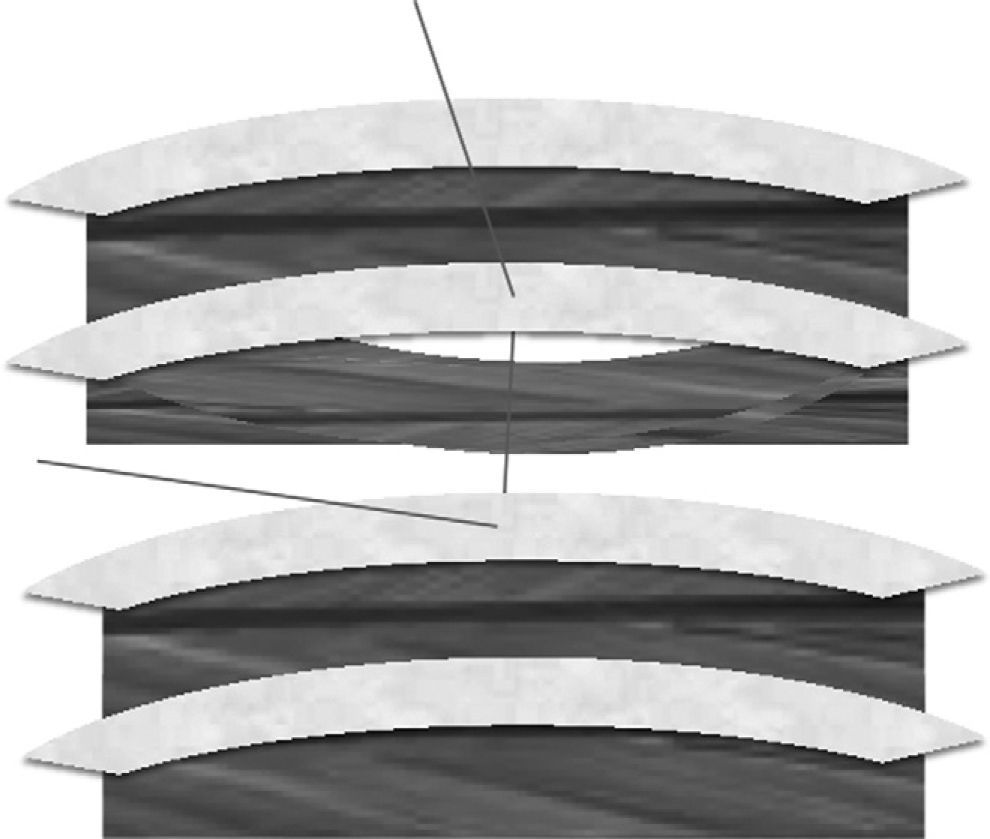
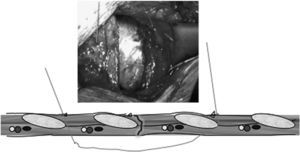
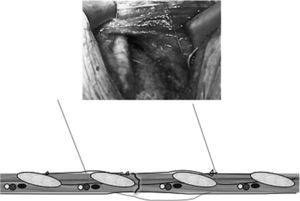
In 2003, this same author described a technical modification in the classic suture of the intercostal space: perform the suture through the rib (transcostal or intracostal sutures)10 (Fig. 2). The traditional suture, unlike this modification, goes around the ribs that are craneal and caudal to the thoracotomy space (Fig. 3).
Combining both technical modifications described by Cerfolio, the study includes 120 patients who underwent posterolateral thoracotomy.11 They were randomized into two groups: one in which separation was carried out with the flap technique and intracostal suture, and the other group in which pericostal suture was done; each of the groups was made up of 60 patients. The authors compared the surgery time, rib fractures, post-op lung function, time until walking, pain medication taken in the first week, dose of epidural catheter analgesia, drainage time, post-op complications, hospital stay, normalization of daily activities, as well as the pain medication and analgesia used 1, 3 and 6 months post-thoracotomy. The groups treated with intercostal flaps and intercostal sutures had significantly less pain during the first week, started to walk earlier, faster return to normal life and less consumption of analgesia. After one month, this significant difference was maintained with regards to pain, although both groups were equal after 3 months. However, the group managed with flaps and intercostal sutures maintained a significantly lower consumption of analgesia. Six months later, there were no differences between the two groups. The study, formally well designed, compared a technique combining analgesic elements in opening and in closing with classic pericostal suture. In this direction, it cannot be established if the beneficial effect in the registered parameters (with special interest given to pain measurements) is due to the opening technique, the suture technique, or the use of both together.
However, in a recently published randomized prospective assay, Wu et al.12 compare the effect of intracostal suture with intercostal flaps. The study included 80 patients from 144 consecutive patients undergoing lung resection; 8 were excluded. A total of 72 patients were randomized for inclusion in the group receiving the flap technique in the fifth intercostal space with intracostal suture through the sixth rib. The remaining patients were sutured with intercostal suture through the sixth rib as a single analgesic measure. All patients were managed with epidural catheter, which was withdrawn 24h after surgery. Pain was evaluated daily in all the patients by means of a numerical scale for the first 7 days, after 2 weeks and after 12 weeks. It was measured while patients were resting and during coughing. The consumption of oxycodone was quantified and the intercostal dermatomes affected by hyperesthesia were observed. No significant differences were found between the two groups when evaluating pain at rest or while coughing, nor throughout the study period. Neither were any differences found in the consumption of oxycodone or in the number of dermatomes affected. The study, randomized and with a wide series of patients, concludes that the use of intercostal flaps for the application of the spreader does not provide any improvement in either acute or subacute pain control over suture with intracostal stitches. It is a well-designed study, with sufficient statistical power, although the blinding technique was single-blind. It was not able to evaluate the effects on chronic pain due to the relatively short follow-up period.
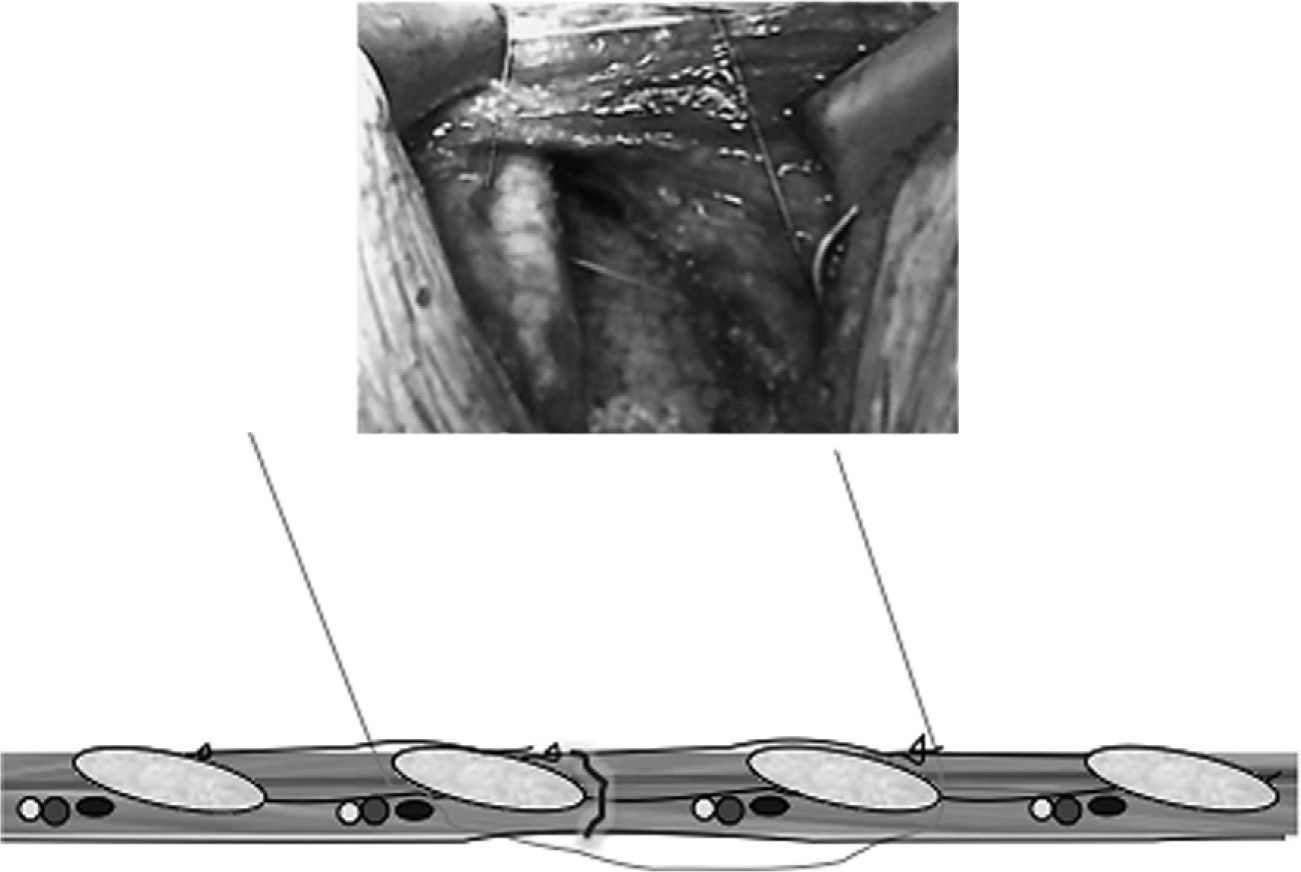
Intercostal Space Suture TechniqueThere is a greater concentration of articles dealing with this aspect of thoracotomy as a factor directly involved in the development of post-thoracotomy pain, although only one is a randomized study. This randomized study is also the most recent, published electronically in 2010 (still in press).13 It compiles 60 patients who underwent posterior mini-thoracotomy with muscle separation. In half of the patients, the intercostal space was sutured with intracostal sutures (Fig. 2). The other 30 patients were sutured in such a way that the intercostal muscle of the thoracotomy space was partially moved out of the way of the suture; here, the cephalic and caudal ribs of the thoracotomy were drilled for a transcostal passage of the suture. The suture went through the cephalic rib, going above the muscle and therefore above the intercostal nerve bundle, avoiding its compression. At the level of the caudal rib, the suture was also intracostal (Fig. 4). Pain was evaluated in both groups with three pain scales (analogical-visual, observer verbal order scale, and Ramsay's) over the course of the first 48h. The difference in favor of the second group was statistically significant (where any sort of intercostal compression was avoided), except on the Ramsay scale, with which no differences were observed. This study provides another interesting technical variation, directed at the key factor for avoiding any type of compression of the intercostal bundle. Nevertheless, the study makes an evaluation of acute post-op pain, but does not provide a follow-up that enables us to evaluate the incidence of chronic pain development.
Another very recent study retrospectively reviewed a series of 184 consecutive patients who underwent posterolateral or anteroaxillary thoracotomy.14 In 141 patients, posterolateral thoracotomy was carried out and in 43 the anteroaxillary method was used. In total, 87 patients received a classic intercostal space suture (Fig. 3), while in 97 patients a technical modification was used (guiding the suture immediately caudal to the lower rib of the thoracotomy space, passing between the rib and the neurovascular bundle, avoiding its compression) (Fig. 5). Pain was evaluated by means of a numerical scale by post-op time periods (1 to 2 weeks, 2 weeks to 1 month, and from 1 to 2 months, 2 to 4, 4 to 6, 6 to 9, and 9 to 12 months). During the one-year follow-up, the patients with posterolateral thoracotomy experimented more pain than those subjected to an anteroaxillary approach. In the same manner, the patients with modified suture had significantly less pain than those who had conventional suture. Collaterally, in 72 patients with posterolateral thoracotomy, intercostal flaps were performed before placing the rib retractor. In this subgroup, there was also a non-significant observed tendency towards experiencing less pain during the first month compared with patients in the same group in whom flaps had not been carried out. The results, although interesting, are not very evaluable: it is a retrospective, not randomized, study where two different approach methods are mixed with two different suture techniques, and even with two different openings within one of the approach types. All this may decidedly bias the validity of the results.
The aforementioned study by Cerfolio published in 200310 which describes and analyzes the results with the intracostal suture technique, is a cohort study that compiles 280 consecutive patients who underwent thoracotomy due to indication for lung resection, excluding patients with chronic pain prior to surgery. In all patients, the same anesthesia and analgesia techniques were used as well as the same technique for performing thoracotomy. The first 140 patients received conventional pericostal suture of the intercostal space (Fig. 3) and the following 140 patients were sutured with intracostal sutures (Fig. 2). Pain was evaluated by means of a numerical scale and the McGill pain questionnaire after 2 weeks and 1, 2 and 3 months post-op. The patients were stratified by age, sex, race, type of lung resection, number of pleural drains, number of costal orifices, time of pleural drainage and hospital stay, observing that there were no differences between groups. The difference in pain after 2 weeks and 1, 2 and 3 months was statistically significant in favor of the group sutured with intracostal sutures. The difference in the perception of quality of pain was also significant: the patients sutured with pericostal sutures described it as being more burning, shooting or sharp. This study, although non-randomized, compares two statistically analogous groups, managed peri- and postoperatively in the same way, with the difference of the thoracotomy closure technique used. The number of patients is considerable, which gives it more statistical power. Therefore, it is a solid study, with very significant conclusions that leave no room for doubt of the thoracotomy closure technique recommendable for the prevention of post-thoracotomy pain.
The rest of the articles related with the thoracotomy closure technique and post-thoracotomy pain provide a lower level of evidence. One of them is a prospective experimental study in animal experimentation.15 The authors carried out a first phase in 2 canine cadavers, evaluating the incidence of entrapment of the intercostal nerve with 4 varying techniques for passing the intercostal suture with pericostal stitches: (a) first of all, passing the tip of the needle immediately under the caudal rib; (b) passing the mandrel of the needle first immediately under the caudal rib; (c) firstly passing the tip of the needle, staying away from the edge of the caudal rib; and (d) passing first of all the mandrel of the needle, staying away from the edge of the caudal rib. In a second phase, pain was evaluated after intercostal suture with the pericostal technique (by passing the mandrel of the needle near the edge of the caudal rib) (7 dogs) and after intracostal suture (6 dogs). The measurement was done with pain threshold scales, rates of fentanyl administration, cardiac and respiratory parameters, and numerical scale of conduct. The pain threshold was measured by an observer who did not participate in the closure of the thoracotomy, 2, 4, 12 and 24h post-thoracotomy, and fentanyl was administered by a second observer, who was also not involved in the closure of the thoracotomy, according to his/her impression of the animal's comfort.
As a result of the first phase of the study on cadavers, an incidence of nerve entrapment of 70% was found in the modality that included first passing the mandrel of the needle immediately under the caudal rib. With the remaining variations of pericostal sutures, 100% entrapment of the intercostal bundles was observed. The pain threshold scale was significantly higher and the rate of fentanyl lower in the group treated with intracostal stitches during the first 24h post-op. The paper shows, experimentally, the anatomic compressive effect that the pericostal sutures exert on the intercostal bundle, confirming a lower level of pain in the immediate post-op period with an intercostal suture technique that avoids this compromise. This experiment corroborates the pathogenic implication of the type of suture used, although the number of animals included is limited and the study only analyzed the effect on immediate post-thoracotomy pain (24h), an excessively short period of time.
Another of the contributions found in the review of the literature is a letter to the editor from 200516 concerning the article by Cerfolio published in 200310 about intracostal sutures. The authors state having used the technique prior to the publication of the study, accompanied by opening with intercostal flaps. They do not analyze their experience, but they communicate their impression of how favorable this technical conjunction is in the post-operative pain of their patients. It is uncommon, but they do comment on the risk for post-surgical pulmonary hernia as a failure of the technique, based on their own experience in one case. The response by Cerfolio admits that the technical description is not new, but that its contribution was to demonstrate the effectiveness of the technique in controlling post-op pain. Likewise, he admits the use of the procedure of intercostal flaps when opening by many surgeons in order to avoid the compression of the intercostal nerve, although this had not been demonstrated until that time. In this context, Cerfolio discusses the development of a randomized prospective study that his group had carried out, which was being published, about the effectiveness of intercostal flaps prior to the placement of the rib spreader. In short, it does not provide a significant contribution about the suture technique and post-thoracotomy pain, aside from the impressions of the authors of the letter and the responses of the author of the clinical assay mentioned.
Finally, there is a technical note that appears in the literature in 2002 about an alternate technical variation for closure of the thoracotomy17 using horizontal mattress stitches between the intercostal muscles. The authors clarify that the technique is only valid for mini-thoracotomies with small intercostal openings. They speculate with the physiopathological reasoning that it avoids the compression of the intercostal bundle and they hypothesize about its possible beneficial effect on post-operative pain, without providing data to support this.
ConclusionsThe following is an analysis of the level of evidence of the publications found in the literature about thoracotomy closure techniques and their relationship with post-thoracotomy pain, using the levels of evidence of the Oxford Center for Evidence-Based Medicine (OCEBM)18:
- 1.
With regards to the use of absorbable osteosynthesis material and its relationship with post-thoracotomy pain, it seems that the use of resorbable osteosynthesis plates may be better than the classic pericostal suture technique, although this finding is not statistically significant.8 Despite the fact that it is a randomized clinical trial, it has only been published as a communication at a congress. Therefore, it cannot be assigned a level of evidence.
- 2.
The use of resorbable osteosynthesis needles significantly reduces post-thoracotomy pain inmediately6,7 and after 1, 2 and 6 months,6 although the studies present few cases. Level of evidence: grade B, level 2b.
- 3.
The conjunction of performing intercostal flaps in order to avoid compression by the rib spreader with an intracostal suture technique is significantly more effective in immediate pain control than classic pericostal sutures,11 maintaining the effect one month after surgery. Three months later, the perception of pain is equivalent, maintaining a significantly higher consumption of analgesics in the pericostal suture group. The differences disappear after 6 months. Level of evidence: grade A, level 1b.
- 4.
Nevertheless, the intercostal flaps for the application of the spreader do not provide better acute or subacute pain control when compared with sutures with intracostal stitches.12 No significant differences were found in the evaluation of pain either at rest or while coughing (throughout the study period), nor in the consumption of oxycodone or in the number of dermatomes affected. Level of evidence: grade A, level 1b.
- 5.
Intracostal sutures with removal the intercostal muscle for the passage of the superficial suture to the intercostal plane are significantly more effective in acute post-operative pain control (48h) than intracostal suture without removal.13 Level of evidence: grade A, level 1b.
- 6.
The intercostal suture with passage of the stitch between the lower edge of the caudal rib of the thoracotomy and its intercostal bundle significantly reduces post-thoracotomy pain in the first year compared with classic pericostal suture.14 Level of evidence: grade C, level 4.
- 7.
Intracostal sutures control post-op pain significantly better, both immediately and after 1, 2 and 3 months, than classic pericostal suture.10 Level of evidence: grade A, level 1b.
- 8.
Pericostal sutures have a high risk for entrapment of the intercostal nerve, conditioning an immediate post-op pain that is significantly greater than with intracostal suture (non-compression technique).15 Level of evidence: grade B, level 2c.
There is very little scientific evidence on certain technical aspects of intercostal space sutures and post-thoracotomy pain. Recommendations can only be established in this regard based on unique studies, with a higher or lower level of evidence depending on their design. The common aspect of all of them is the importance given to the preservation of the intercostal nerves. It is necessary to develop a randomized prospective study that specifically compares the different technical variations for thoracotomy closure described in the literature and their relationship with post-thoracotomy pain.
FundingThis review received no funding of any type.
Conflict of InterestsThe authors declared that they have no conflict of interests.
Please cite this article as: García-Tirado J, Rieger-Reyes C. Técnica de cierre de la toracotomía y su relación con el dolor postoracotomía: revisión sistemática. Arch Bronconeumol. 2011;48:22–8.