Pneumonitis due to hypersensitivity to wood fiber is mainly associated with the fungus that colonizes it. We present the case of a male affected with hypersensitivity pneumonitis in which the agent implicated was medium-density fiberboard, an engineered product whose main component is pine wood fiber. The causal agent was identified by means of a specific bronchial provocation test.
La neumonitis por hipersensibilidad en relación a maderas se asocia principalmente a los hongos que las colonizan. Presentamos el caso de un varón afecto de neumonitis por hipersensibilidad en el que el agente implicado fue una madera de densidad media, producto industrial cuyo principal componente es la madera de pino. La identificación del agente causal se realizó por medio de una prueba de provocación bronquial específica.
Hypersensitivity pneumonitis (HP) is a disease that is characterized by an abnormal immune reaction to the exposure to different antigens over a prolonged period of time, and its immunopathogenesis is related with delayed hypersensitivity mediated by T-cells.1,2 Although there is an association between this pathology and certain occupations, it is not a disease that entails mandatory reporting and therefore its prevalence and incidence are difficult to estimate.3 One of the occupations involved in the genesis of this disease has been carpentry. In this regard, although some reported cases have demonstrated that the antigens of the wood itself are the causal agent,4,5 usually it is the fungi that colonize the wood that are responsible for the disease.6–9
We present the case of HP in a carpenter in whom the agent involved was medium-density fiberboard (MDF), an industrial product that is a variation of particle board.
Case ReportThe patient is a 37-year-old male, with no toxic habits and with no known pathological history. As a professional carpenter since the age of 16, he has been in contact with mainly MDF, and usually has not used protection while working.
The patient complained of dry cough, dyspnea, low-grade fever, chest pain, arthromyalgia and persistent asthenia over the last 7 years. Said symptoms improved while the patient was on vacation.
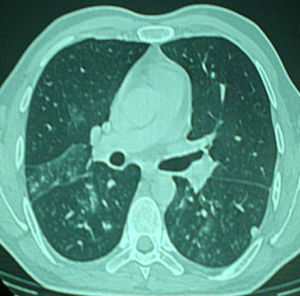
The physical examination was normal, and the general work-up showed no relevant findings. Lung function studies showed a forced vital capacity (FVC) of 4.94 l (91%), forced expiratory volume in 1s (FEV1) of 3.96 l (93%), FEV1/FVC ratio 80%, residual volume (RV) 80%, total lung capacity (TLC) 91%, carbon monoxide diffusing capacity (DLCOsb) 75% and (DLCOva) 88%. Both the bronchodilator test and the non-specific bronchial provocation test with methacholine were negative. Chest computed tomography (CT) showed a micronodular pattern with patchy areas of ground glass (Fig. 1).
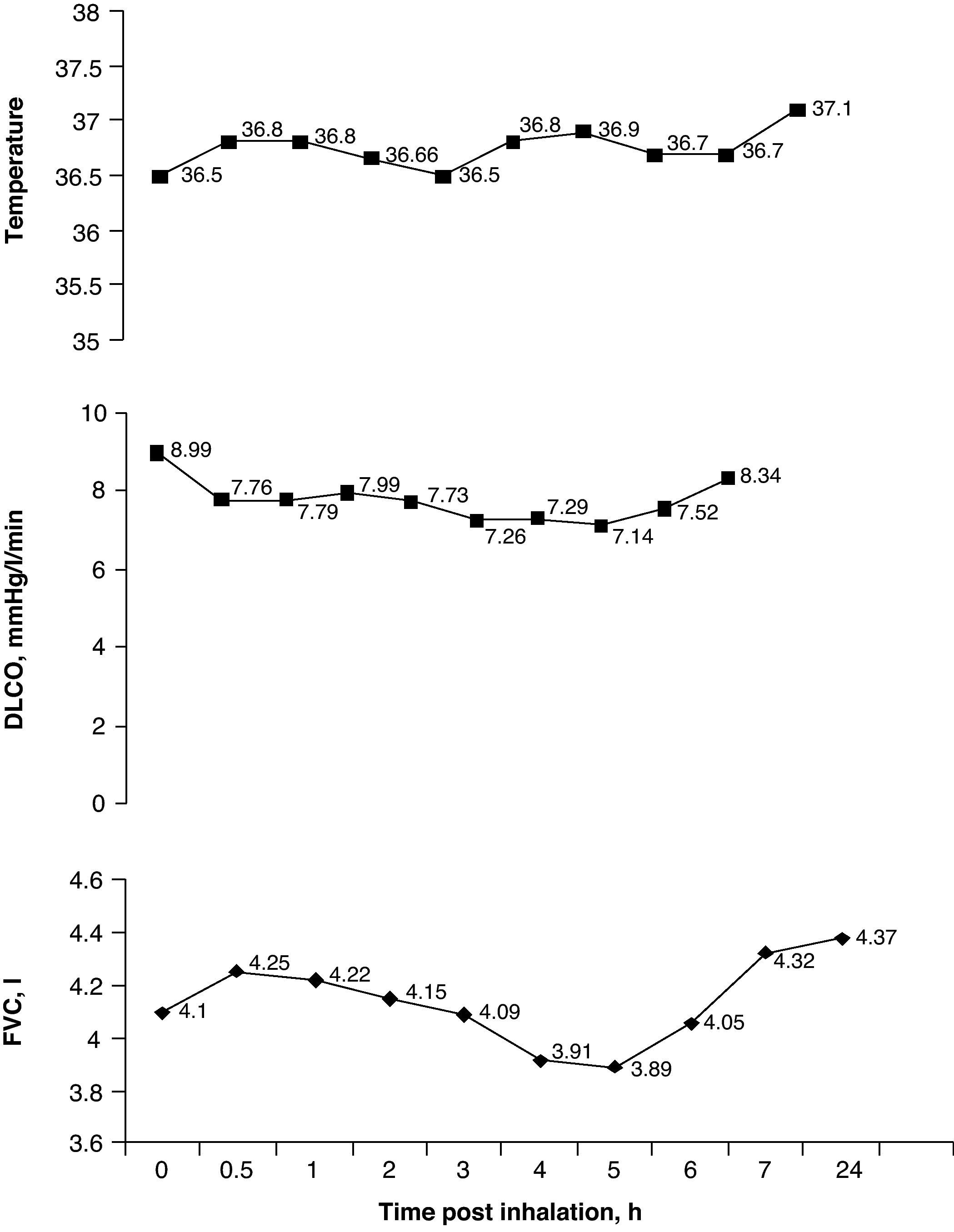
The culture of the wood responsible for the patient's symptoms was positive for Candida sp. The immediate skin reaction tests for Candida sp., Penicillium frequentans and Aspergillus fumigatus were negative. The determinations of G immunoglobulin by means of the ELISA technique for Candida sp., P. frequentans and A. fumigatus were also negative. A specific bronchial provocation test (BPT) with a commercial Candida sp. extract, performed following the recommendations proposed by our group,2 was negative. A second BPT with direct exposure of the patient to the wood product in question in a provocation booth for 60min was positive after confirming a decrease in FVC of 15% and in DLCO of 21% with an increase in temperature of 0.6°C, going from 36.5 to 37.1°C and starting 5h after the beginning of the exposure (Fig. 2). None of these changes were observed when the patient was exposed to a placebo the previous day. Twenty-four hours after the exposure, bronchoscopy with bronchoalveolar lavage (BAL) demonstrated a cell count with 80% macrophages, 18% lymphocytes and 2% polymorphonuclear cells.
Specific bronchial provocation test (BPT) against medium-density fiberboard (MDF). The test was considered positive with an observed decrease in FVC of 15%, a decrease in DLCO of 21% and an increase in temperature of 0.6°C. DLCO: carbon monoxide diffusing capacity; FVC: forced vital capacity.
After the exposure, the patient remained asymptomatic, and the thoracic CT as well as the different lung function studies normalized.
DiscussionWe report the case of a patient with HP to MDF wood, an industrial product that is a variation of fine-particle board whose main component is pine wood. The clinical symptoms that the patient presented, as well as the radiological findings and a mild reduction in the CO diffusion test, suggested the diagnosis of HP. As the patient clearly related the symptoms with the exposure to MDF, BPT was then carried out in order to both ensure the diagnosis and establish the causal agent. The disappearance of the symptoms and the normalization of the radiology after the exposure confirmed the diagnosis.1,2 The fact that the wood culture was only positive for Candida sp., that the immunological tests were negative for the different fungi tested, and that the provocation test was positive for MDF sawdust and not for Candida sp. extract all suggest that the wood itself is the cause of the patient's illness.
In general, when a patient in contact with wood is diagnosed with HP, the etiological agent is usually a fungus. There are certainly references in this direction, and the most frequently involved fungi are Aspergillus species, Penicillium species, Cryptostroma corticale, Alternaria, Graphium, Aureobasidium pullulans, Mucor sp. and Trichoderma spp.6–10 We have not found any references relating Candida sp. as a causal agent of HP related to wood exposure, although it is known to be related to the use of humidifiers.11–13
There are also cases in which the wood itself has been identified as the causal agent. The types of wood implicated are red cedar, iroko, ramin, oak and mahogany.14 In general, the diagnoses were established by BPT and by determination of specific antibodies against wood extracts. Our group has also been able to demonstrate the involvement of cork wood as a cause of HP. After studying eight patients with suberosis by determining specific IgG antibodies and carrying out skin tests and BPT for cork and different fungi, it was demonstrated that the only causal agent was the cork itself in at least one patient, while its involvement was not clear in another two patients.5
Recently, Malmstrom et al.4 have demonstrated a response of specific IgG antibodies to pine carbohydrates in a patient with HP, suggesting that said compositions could also be involved in the genesis of this entity. Said authors ruled out the fungal etiology although no specific bronchial provocation test was done. In this sense, we cannot exclude that the origin of the HP of the patient that we have presented here may be the exposure to said molecules, keeping in mind that the main component of MDF is pine wood.
In conclusion, after excluding the fungal etiology of this HP, we can affirm that it is caused by the MDF itself. We believe in the relevance of this contribution as these wood products are currently widely used in our society.