The established endoscopic treatment of web-like tracheobronchial stenosis is laser vaporization, but the appearance on the market of a new cutting mode with a lower coagulation effect has been proposed as an alternative to laser due to less injury to the tissue.
ObjectivesTo study the clinical and functional consequences, as well as the side effects of this technique. Afterwards, we investigated whether the use of an electrosurgical knife with this technique is as effective and convenient as an ND-YAG-laser.
Patients and methodsBetween March 2005 and July 2007, included for study were 22 patients who had undergone 34 interventional bronchoscopy procedures with the VIO-300-D radiofrequency system, using a mode of the Endo-cut I program in conjunction with the reusable knife electrode.
ResultsAll of the patients treated (100%) presented improvements in their symptoms, in the tracheobronchial lumen diameter and in lung function, which were statistically significant. Symptom-free time was 157±93 days. There was an overall decrease observed in mean obstruction (P<.001). Improvements in FVC (P=.01), raw (P=.0016) and RV/TLC (P=.01) were significantly significant. Less than 50% of the patients needed a second intervention.
These patients were compared retrospectively with a similar group of 22 patients treated with Nd-YAG laser. The follow-up analysis showed that only 18% (4/22) of the patients treated with this new technique presented fibrin, compared with 41% (9/22) of those treated with laser therapy (P<.001).
ConclusionThe use of this technique is effective for the treatment of benign web-like tracheobronchial stenosis as all the patients showed clinical and functional improvement, and less than 50% required a second intervention. In comparison with laser therapy, an advantage of this technique is that less fibrin is produced, probably due to the reduced anti-coagulation effect.
El tratamiento endoscópico establecido de las estenosis traqueobronquiales tipo web-like es el láser. La aparición en el mercado de un nuevo modo de corte con un menor efecto coagulante, se ha postulado como una alternativa al láser debido a un menor daño en los tejidos afectados.
ObjetivosEstudiar las consecuencias clínicas, funcionales y los efectos secundarios de esta técnica y posteriormente compararla con un grupo similar de pacientes tratados con láser ND-YAG.
Pacientes y métodoEntre marzo del 2005 y julio del 2007 se incluyeron 22 pacientes que fueron sometidos a 34 procedimientos de broncoscopia intervencionista mediante el sistema de radiofrecuencia VIO-300-D, usando un modo el programa Endo-cut I en combinación con el electrodo de cuchilla reutilizable.
ResultadosEl 100%de los pacientes tratados presentaron una mejoría de los síntomas, del diámetro de la luz traqueobronquial y de la función pulmonar que fueron estadísticamente significativos. El tiempo libre de síntomas fue de 57±93 días, necesitando menos del 50% de los pacientes una segunda intervención.
Retrospectivamente, se compararon estos pacientes con un grupo similar de 22 pacientes tratados con el láser Nd-YAG. El análisis de seguimiento mostró que sólo 18%(4/22) de los pacientes tratados con esta nueva técnica presentaron fibrina en comparación con el 41%(9/22) de los tratados con láser (p<0,001).
ConclusiónEl uso de esta técnica es eficaz en el tratamiento de las estenosis benignas traqueobronquiales tipo web-like ya que todos los pacientes mostraron mejoría clínica y funcional, requiriendo menos del 50% una segunda intervención. En comparación con el láser, una ventaja de esta técnica es la menor producción de fibrina, probablemente debido a su menor efecto anticoagulante.
Benign stenoses of the trachea and bronchi are still a relevant clinical problem. Said stenoses have different causes, and the most frequent etiologies are prolonged intubations, toxic inhalation, chest trauma, tracheobronchial tuberculosis, after lung transplantation or other less frequent causes, such as polychondritis and systemic diseases like Wegener's granulomatosis or amyloidosis. In addition, cicatricial stenosis can develop in patients diagnosed with lung cancer who receive treatment with radiotherapy or endobronchial brachytherapy.1–6,17
Currently, tracheobronchial stenoses are divided into: (a) web-like stenosis or diaphragm stenosis caused by circumferential erosion of the mucosa that cause concentric stenosis without damage to the mucosa and (b) complicated stenoses, which are stenoses of more than 1cm, with irregular edges and that are associated with different degrees of tracheomalacia. The early diagnosis of these stenoses is key, as the majority of patients can benefit from therapeutic interventions that may alleviate their symptoms and in this way prevent future complications.7
The initial symptoms are usually cough and dyspnea, like in other respiratory pathologies; therefore, a detailed patient medical history is of vital importance for orienting the diagnosis. Depending on the degree of stenosis, it is possible that stridor may appear. If the stenosis is not treated early, the patient may develop post-obstructive pneumonia, atelectasis and even respiratory arrest and death.6
So, although the symptoms and the clinical history should guide the diagnosis, the definitive diagnosis should include imaging or endoscopic techniques. The procedure of choice is bronchoscopy, as it enables one to see the type of stenosis, its location and degree.7,8
The therapeutic regime depends on the type of stenosis and its extension.6–8 Diaphragm or web-like stenosis requires a completely different type of treatment than complicated hourglass stenosis. In the case of idiopathic tracheal stenosis measuring less than 2cm located in the upper third of the trachea, the treatment of choice is resection of the stenosis and end-to-end anastomosis.1,2 However, surgical interventions carry with them associated morbidity and mortality and possibilities for relapse of the lesion. Therefore, in recent years new alternatives with endoscopic treatments are being explored.6–8 The progressive appearance of endobronchial treatments (laser, electrocautery, argon plasma coagulation) has been gaining popularity due to the limited adverse effects and the low incidence of morbidity and mortality that they present, together with the possibility for cure in a subgroup of patients.10
In oncologic patients, the objective is to improve the symptoms and, consequently, quality of life. Nevertheless, in the case of endobronchial treatment of benign stenoses, it is considered that the treatment is a success if we are able to achieve that the patient remains asymptomatic during long periods of time with few or minimal adverse effects.6–9
In the case of endoscopic treatment of benign stenoses, there are therapies like pneumatic tracheal dilation, electrocautery and laser11–15 that are accepted, as they have demonstrated their usefulness. In the case of web-like benign stenoses, laser treatment has been established as the endobronchial treatment of choice,12 although in recent years electrocautery has become its rival due to its lower cost.8 However, it is well-known that these thermal sources can produce fibrin plates, necrosis and granulomas. These side effects produce frequent local re-stenosis, which mean having to repeat the therapeutic procedures.10–15 The appearance on the market of a new cutting mode is purported to be an alternative to laser because it has less side effects.
As for the instruments used, currently there are only limited data on the use of the re-usable electrode knife (also known colloquially among bronchoscopists as endobronchial scalpel) for the treatment of benign web-like stenoses of the tracheobronchial tree. Neither the effectiveness nor the safety of this instrument has been evaluated prospectively.2,7–9 In this article, in addition to describing the use of said instrument and following-up the patients, we describe for the first time the use of a surgical radiofrequency system (VIO-300-D, ERBE, Germany) together with a novel and optimized intermittent cut mode for the treatment of benign web-like stenoses of the trachea. Furthermore, it is the first study to describe the use of a new isolated-tip electrode knife, with which we guarantee damaging no part of the unaffected airway, which on occasion is difficult to visualize due to the small diameter afforded by the stenosis.
The main objective of this study is to present our experience in the treatment of web-like tracheobronchial benign stenoses using the endobronchial scalpel with the VIO 300 generator (ERBE, Germany), with its optimized cut mode (Endo-cut I), taking into account clinical and functional results as well as possible complications and side effects. Retrospectively, the side effects of this new technique were compared with patients treated with ND-YAG laser.
Patients and MethodsWe carried out an observational prospective study after the protocol had been previously approved by the ethics committee of the Hospital Lungenklinik Hemer (Hemer, Germany). All the patients gave their informed consent and consent for the inclusion of their data in this present study.
Included in the study were all those patients with benign stenosis of the trachea who were remitted to our interventional pulmonology unit, part of the Pulmonology Department of the Hospital Lungeklinik Hemer, between March 2005 and July 2007. Those patients who had been diagnosed endoscopically with web-like cicatricial stenosis (according to the airway stenosis classification system by Dr. Freitag7) were offered the possibility to participate in the study. The procedure was considered a success if no new interventions had to be performed in the following 6 months. The side effects of this technique were compared with the follow-up bronchoscopies that were done in a group of patients with similar initial characteristics who had been treated with laser.
Inclusion and Exclusion CriteriaWe selected patients over the age of 18 with benign stenosis of the tracheobronchial tree, diagnosed by bronchoscopy, who met with the following criteria: symptoms secondary to tracheobronchial stenosis, benign trachea stenosis and web-like bronchial stenosis with no contraindications for doing rigid bronchoscopy. Patients with malignant stenosis, those with pacemakers and patients who were candidates for surgical resection were excluded.
ProcedureThe procedure was done according to the standard protocol of our hospital for interventionist bronchoscopy. Rigid bronchoscopy was done in all cases under general anesthesia with an initial bolus of propofol at 2mg/kg and remifentanil at 1μg/kg. Later, an intravenous perfusion of propofol (0.2μg/kg/min) and remifentanil (0.25μg/kg/min) was used. For muscle relaxation, mivacurium was used at a dose of 0.1mg/kg. The patients were constantly monitored with electrocardiogram, blood pressure and oxygen saturation. Once the patients were intubated with a tracheoscope or rigid bronchoscope, bronchoscopy (Olympus, Japan) was performed with a rigid bronchoscope (Wolf, Germany). The patients were ventilated with jet ventilation, using the Mistral respirator (Acutronic, Hirzel, Switzerland). During the activation of the electrocautery, the inspiratory fraction of oxygen (FiO2) was lowered to below 0.4 to prevent ignition in the airway.
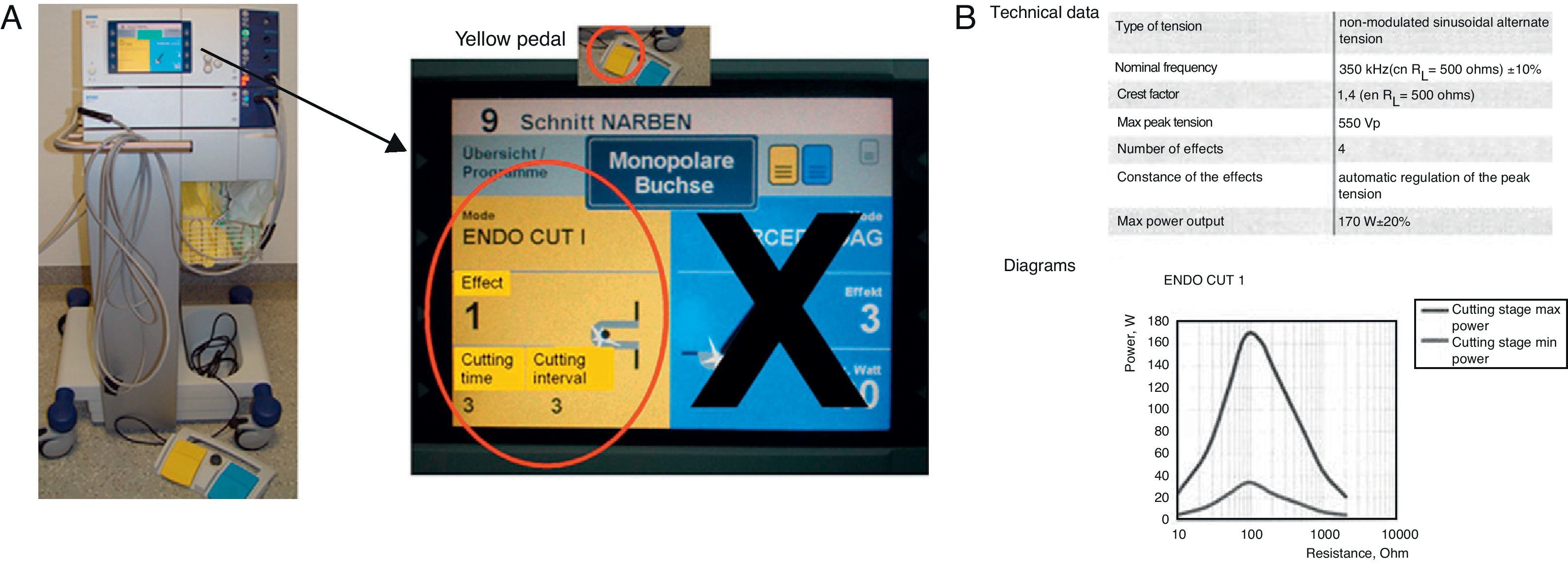
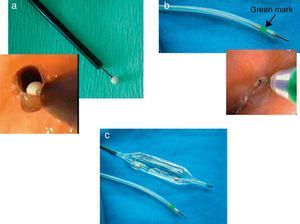
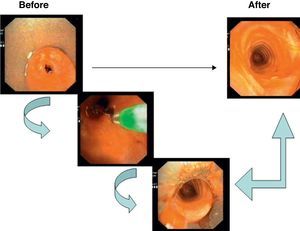
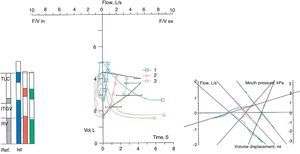
The treatment of the stenosis itself was done with an endobronchial scalpel connected to a VIO-300-D (ERBE, Germany) high-frequency current system. This device has different programs designed for different instruments and clinical problems; in our case, we used the Endo-cut I program (Fig. 1). Previously, a neutral electrode (NESSY Omega-ERBE, Germany) was placed on each patient in order to close the electrical circuit and for the monopolar cutting instrument to activate. With the Endo-cut I program, different cutting effects can be selected with different degrees of coagulation. The cutting interval (coagulation time between the two cutting phases) presents a scale from 1 (very short) to 10 (very long interval). The duration of the cut also varies from 1 to 4 (4 is the longest cut). Based on previous in vitro experiments, we opted for the following configuration: coagulation effect 1, cutting interval 3 and cutting time 3. With this program, a well-controlled, soft cut of the stenoses was documented.
The power of the Endo-cut I is adjusted by adjusting the effect, the duration of the cut and the interval of the cut. With Endo-cut I, it is not necessary to adjust the wattage or to set an upper power limit because the high-frequency current is regulated depending on the resistance of the tissue. Thus, compared with electrocautery or ICC technology, in which the power is pre-selected, the VIO generator allows for optimal power using an intelligent self-regulating system. In other words, in the VIO generator the electrosurgical current is adjusted automatically depending on the electrical resistance of the tissue. Thus, the range of power is variable and depends on the tissue. The output of the actual power is not indicated on the screen as it depends on the resistance. This means that, with the Endo-cut I combined with the VIO generator, the necessary current is calculated by the VIO generator automatically depending on the resistance of the tissue to be treated (Fig. 1B).
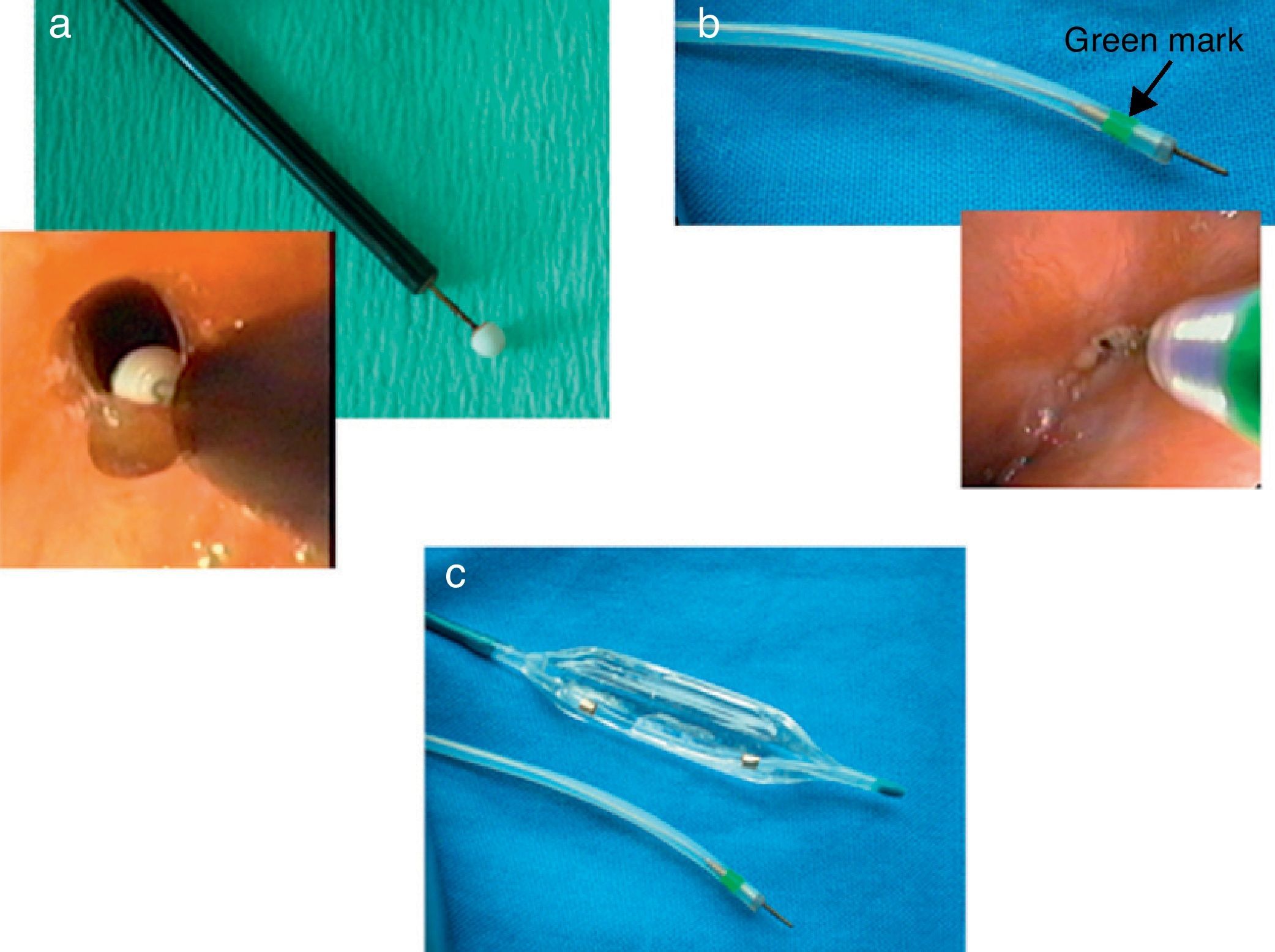
The majority of the patients were treated with the endobronchial scalpel (KD-31C-1, Olympus, Tokyo), which is a scalpel blade with a non-isolated, re-usable tip. New isolated-tip endobronchial scalpel blades (IT Knife KD-610-L, Olympus, Japan, and EMR-Knife 99020271, MTW, Germany) were also used (Fig. 2).
Before performing the procedure, bronchoscopy was done to evaluate the airway and especially to evaluate and measure the longitude of the stenosis. In the case of high-grade stenoses, occasionally pediatric bronchoscopy (BF-P160 ó 3C-160, Olympus, Japan) was necessary in order to pass along the tracheobronchial lumen afforded by the stenosis. It is very important to be able to see the beginning and end of the stenosis in order to ensure a precise cut. Once the stenosis was analyzed, a bronchoscope with a larger working channel (diameter 2.8mm) was used, which was necessary to be able to introduce the endobronchial scalpel.
The scalpel was introduced through the working cannel, after which the scalpel was applied to the lesion. Next, after stepping on the yellow pedal, the current was applied (Fig. 1A), cutting the stenosis with direct vision. In the cases in which the end of the stenosis was not visualized, a cutting electrode with an isolated tip was used to avoid either lesions or burns to healthy areas. As seen on microscope, the spark discharged by the high-frequency current vaporizes the intracellular water and causes the disintegration of the cell. Macroscopically, a clean cut is observed in the tissue. The instrument works by contact and needs to be cleaned repeatedly throughout the procedure in order to obtain optimal performance.
One single cut was generally sufficient although occasionally two cuts were necessary to be able to achieve complete recanalization. Generally, these cuts are done in the direction of the angle that joins the pars membranacea with the pars cartilaginosa, because it is where the greatest recovery of the tracheobronchial diameter prior to the lesion is obtained.
With the intention of obtaining a greater and immediate opening effect, the technique described was combined with the use of dilation balloons (Boston Scientific, USA) (Fig. 2), or instead the tip or bezel of the rigid bronchoscope was used (Fig. 3).
48h after the intervention, the patients underwent clinical evaluation, lung function testing, baseline arterial blood gas and control bronchoscopy with local anesthesia and sedation with midazolam. Photos and videos of the endoscopic images were taken, evaluating the degree of narrowness and the presence of fibrin plates.
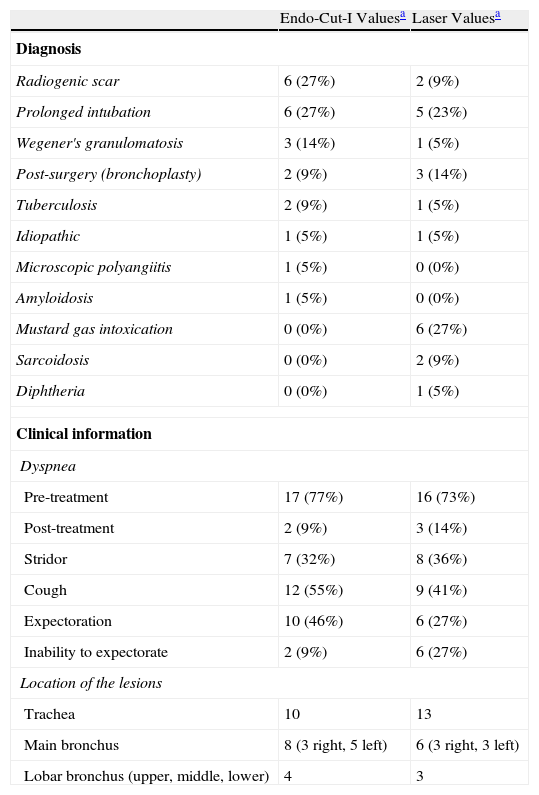
Later, a comparison was done with the reports and recorded images from a group of patients with similar initial characteristics who were treated with laser. Table 1 shows the etiology, clinical data and location of the patients treated with either endobronchial scalpel or ND-YAG laser.
Etiology, Clinical Data and Location of the Stenosis.
| Endo-Cut-I Valuesa | Laser Valuesa | |
| Diagnosis | ||
| Radiogenic scar | 6 (27%) | 2 (9%) |
| Prolonged intubation | 6 (27%) | 5 (23%) |
| Wegener's granulomatosis | 3 (14%) | 1 (5%) |
| Post-surgery (bronchoplasty) | 2 (9%) | 3 (14%) |
| Tuberculosis | 2 (9%) | 1 (5%) |
| Idiopathic | 1 (5%) | 1 (5%) |
| Microscopic polyangiitis | 1 (5%) | 0 (0%) |
| Amyloidosis | 1 (5%) | 0 (0%) |
| Mustard gas intoxication | 0 (0%) | 6 (27%) |
| Sarcoidosis | 0 (0%) | 2 (9%) |
| Diphtheria | 0 (0%) | 1 (5%) |
| Clinical information | ||
| Dyspnea | ||
| Pre-treatment | 17 (77%) | 16 (73%) |
| Post-treatment | 2 (9%) | 3 (14%) |
| Stridor | 7 (32%) | 8 (36%) |
| Cough | 12 (55%) | 9 (41%) |
| Expectoration | 10 (46%) | 6 (27%) |
| Inability to expectorate | 2 (9%) | 6 (27%) |
| Location of the lesions | ||
| Trachea | 10 | 13 |
| Main bronchus | 8 (3 right, 5 left) | 6 (3 right, 3 left) |
| Lobar bronchus (upper, middle, lower) | 4 | 3 |
Data were compiled on patient demographics, diagnoses, symptoms, location of the stenoses, degree of stenosis and complications. The patients were followed-up for at least 6 months. In order to extract statistical data, we classified the stenoses depending on their location and degree of stenosis. The production of fibrin was classified on a two-point scale (0: without fibrin, 1: fibrin plates).
The statistical analysis was done with the SPSS program, version 12.0, for Windows (SPSS Inc., Chicago, IL, USA). The data are presented as mean±standard deviation (SD – range). The Kolmogorov–Smirnov test was used to study the variable distribution. The differences between groups were compared using the Mann–Whitney U-test in the case of variables with normal distribution and the Wilcoxon test in the case of the variables with non-normal distribution. P values <.05 were considered statistically significant.
ResultsBetween February 2005 and June 2007, 22 patients with benign web-like tracheobronchial stenosis underwent 34 therapeutic procedures. Twelve patients (54%) required one procedure, 8 patients required 2 (36%) and 2 patients required 3 procedures (10%).
Twenty-two patients were treated (13 men and 9 women), with a mean age of 54±14 SD (range: 23–72). The etiology of the stenosis, clinical information and location of the stenoses are shown in Table 1. Mustard gas intoxication refers to soldiers who participated in the Iran–Iraq War (1983–1988), in which mustard gas was used, also known as sulfur mustard (bis-[2-cloroetil]), sulfur, yperite (Ypres was where it was first used by the military), LOST (acronym for the German chemists Lommel and Steinkopf, who researched the military use of this chemical composition) and “yellow cross” (German shells were marked with a yellow cross, meaning an agent that was dangerous to the skin). This gas produces, among other toxic effects, eye, skin and respiratory lesions. In the respiratory tract, it may cause many lesions, but the case at hand dealt with patients who presented a severe alteration in the tracheal mucosa with inflammation and necrosis, which caused stenosis in the membrane at the tracheobronchial level.15,16
The procedures were done without any observed immediate or later complications attributable to the technique.
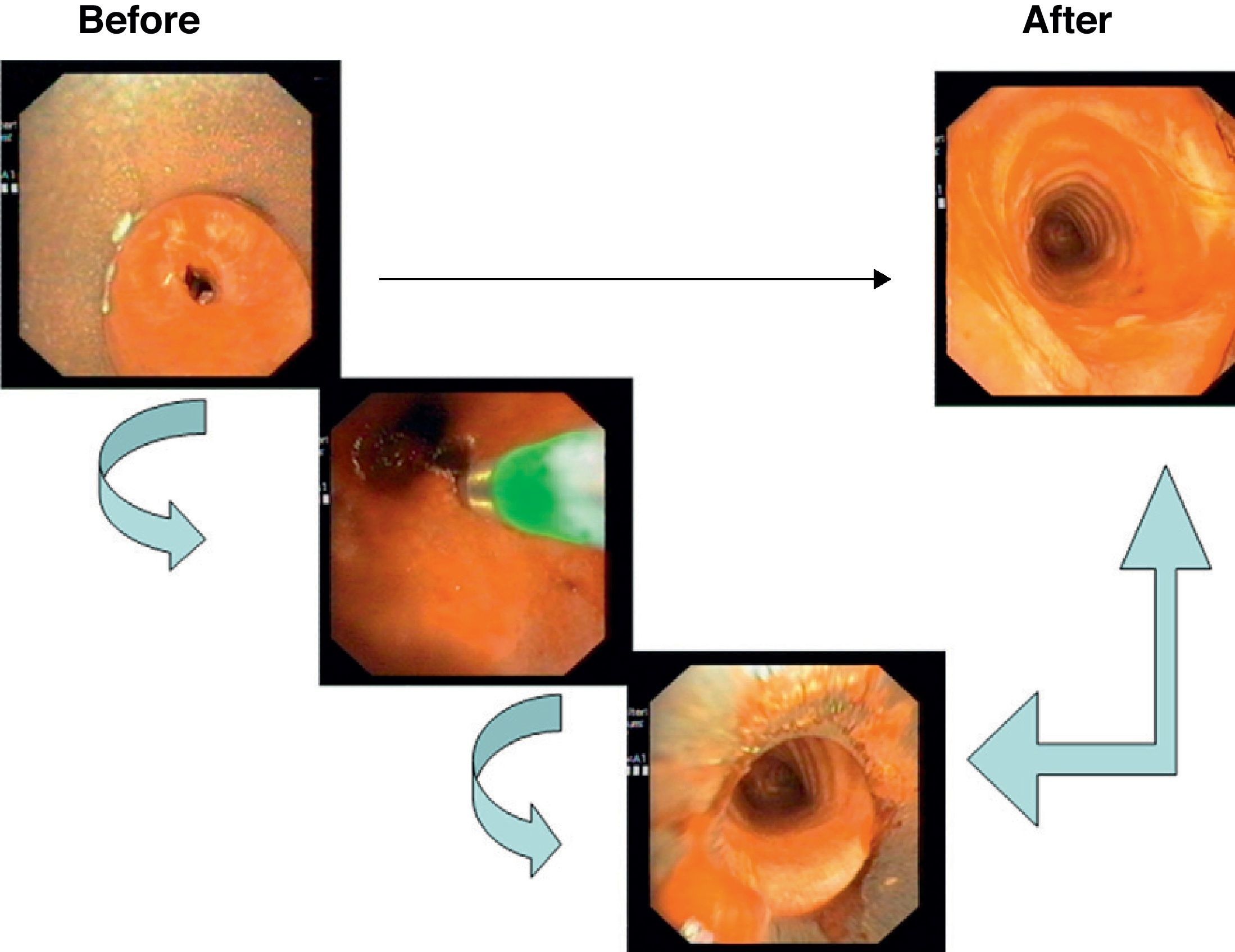
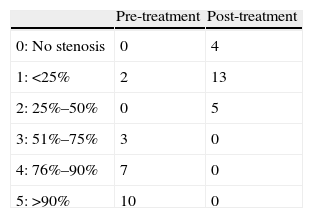
The degree of pre- and post-op stenoses was evaluated visually, taking into account the diameter of the bronchoscope used and the comparison between the stenosis area and the nearby healthy airway, in accordance with the last classification proposed about stenosis of the airway.7 The degrees of pre and post-treatment stenoses were 4.05±1.21 and 1.05±0.65, respectively, with a P<.001 (Fig. 3 and Table 2).
Pre- and Post-treatment Degree of Stenosis.
| Pre-treatment | Post-treatment | |
| 0: No stenosis | 0 | 4 |
| 1: <25% | 2 | 13 |
| 2: 25%–50% | 0 | 5 |
| 3: 51%–75% | 3 | 0 |
| 4: 76%–90% | 7 | 0 |
| 5: >90% | 10 | 0 |
According to the classification of the central stenoses of the airway.7
The control bronchoscope showed minimal fibrin plates, seen in only 4 out of the 22 patients (18%). These findings were compared with the results of 22 patients with web-like stenosis who were treated with ND-YAG laser. In this last group, the control bronchoscopy done between 48–72h after laser showed fibrin plates in 9 of the 22 patients (41%). In addition, 4 of these patients presented formation of tissue with granulomas (P<.001). With regards to the patients treated with the endobronchial scalpel with an optimized cut-mode (Endo-cut I) in which fibrin plates were detected, removal of said plates was not necessary because, rather than plates, these were actually limited lesions in the intervention area. However, out of the 9 patients treated with laser in whom fibrin plates were observed, in 7 patients it was necessary to extract them with flexible forceps as they were circumferential fibrin plates that caused concentric stenosis; in 4 of these patients, a unidirectional valve behavior was observed that produced a sensation of blockage upon inspiration.
The procedure was considered a success if no new procedures were necessary in the following 6 months. Following this criterion, the process was documented as successful in 18 out of the 22 (82%) patients.
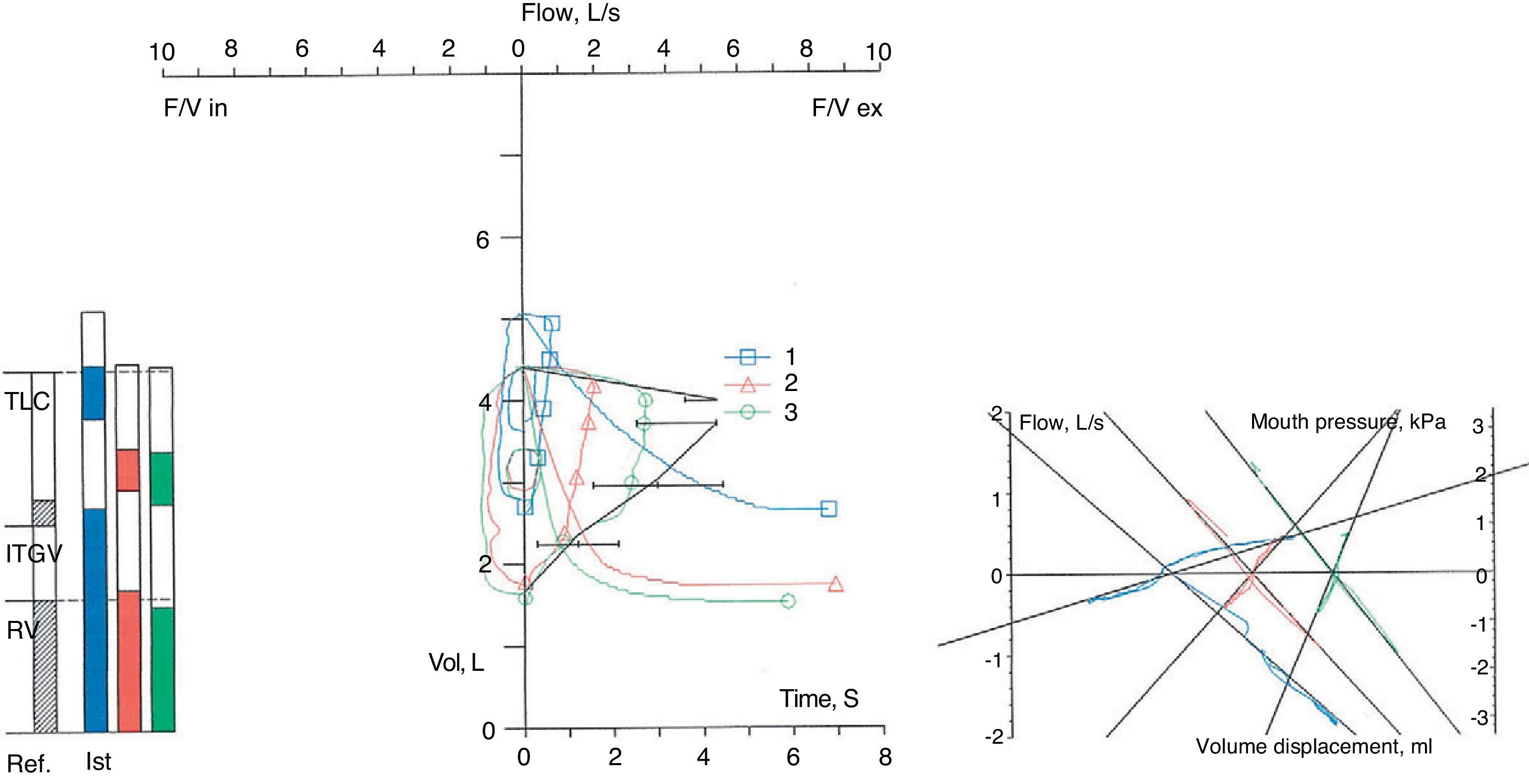
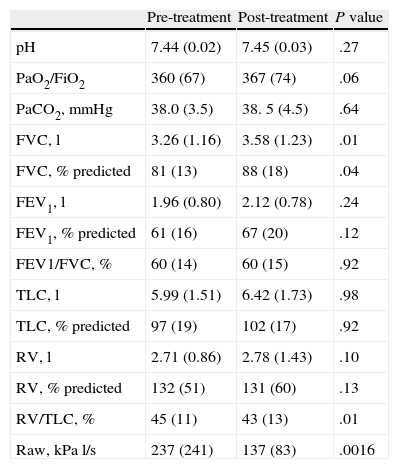
In all the patients treated with the Endo-cut I combined with the endobronchial scalpel when possible (specifically 18 of the 22 patients), baseline blood gas analysis and respiratory function tests were determined before and after treatment (Table 3). Fig. 4 shows the pre- and post-treatment flow-volume curve of a patient with radiogenic stenosis in the upper third of the trachea. These data could not be collected for the patients treated with laser because, as it was retrospective, the majority of the patients had only one complete functional study either previous or posterior to the intervention, but not both.
Baseline Arterial Gasometry and Pre- and Post-treatment Lung Function Tests.
| Pre-treatment | Post-treatment | P value | |
| pH | 7.44 (0.02) | 7.45 (0.03) | .27 |
| PaO2/FiO2 | 360 (67) | 367 (74) | .06 |
| PaCO2, mmHg | 38.0 (3.5) | 38. 5 (4.5) | .64 |
| FVC, l | 3.26 (1.16) | 3.58 (1.23) | .01 |
| FVC, % predicted | 81 (13) | 88 (18) | .04 |
| FEV1, l | 1.96 (0.80) | 2.12 (0.78) | .24 |
| FEV1, % predicted | 61 (16) | 67 (20) | .12 |
| FEV1/FVC, % | 60 (14) | 60 (15) | .92 |
| TLC, l | 5.99 (1.51) | 6.42 (1.73) | .98 |
| TLC, % predicted | 97 (19) | 102 (17) | .92 |
| RV, l | 2.71 (0.86) | 2.78 (1.43) | .10 |
| RV, % predicted | 132 (51) | 131 (60) | .13 |
| RV/TLC, % | 45 (11) | 43 (13) | .01 |
| Raw, kPal/s | 237 (241) | 137 (83) | .0016 |
Values are expressed as means and standard deviation.
PaO2: partial pressure of oxygen; Fi: inspired oxygen fraction; PaCO2: partial pressure of CO2; FVC: forced vital capacity; FEV1: forced expiratory volume in one second; TLC: total lung capacity; RV: residual volume; raw: airway resistance.
As shown in Table 3, the majority of the patients presented improvement in all the lung function parameters, and the forced vital capacity (P=.01), total airway resistance (P=.0016) and ratio between residual volume and total lung capacity (P=.01) were statistically significant.
DiscussionSymptomatic tracheobronchial stenoses require treatment that produces minimal side effects and minimal complications. Ideally, it should be a definitive treatment or at least one with a low rate of recurrences. Web-like cicatricial stenoses can be treated endoscopically with a small incision and dilation techniques. The ND-YAG laser is the established method for this type of stenosis. Argon-plasma coagulation has been considered a safe alternative, but its cutting capacity is limited as it has a low tissue penetration capability, ranging from 2 to 3mm.14,15,18–23
In our study, a more sophisticated device has been used, with a custom program. When the new Endo-cut I cut mode is used with the endobronchial scalpel, its effects are observed to be comparable to those achieved with laser15,18–23 but with a lower production of fibrin, probably due to its lesser penetration and to the fact that the power used depends on the resistance of the tissue to be treated (Fig. 1B). Specifically, what happens with the use of laser is that the deep coagulation damages the blood flow, which reduces the viability of the chondrocytes and alters the re-epithelialization. This tissue damage caused by laser therapy promotes fibrosis, scarring and granulation tissue, and consequently re-stenosis. Both necrosis and the production of fibrin plates are endoscopically visible signs of tissue lesion. Thus, it is reasonable to believe that a lower production of fibrin plates entails a lower risk of re-stenosis.15,18–23
Evaluating these data, statistically significant differences were found in fibrin production in the cases of patients treated with the new cut-mode in comparison with the group of patients treated with laser. Thus, while in the patients treated with the Endo-cut I the production of plates de fibrin was small on the cutting areas and their removal by forceps was not required, in the case of the patients treated with laser the fibrin plates were more considerable in size and required removal with flexible forceps.
An excellent response was obtained with regards to the symptoms, the degree of stenosis and lung function, all probably due to the careful selection of the cases as the ideal candidates for this technique are patients with short (<1cm) web-like benign stenoses who are not candidates for surgery. It is possible that it may be useful in the case of malignant web-like stenoses, but new studies would be necessary in this direction.
The results in the patients with radiogenic stenosis were excellent, with no evidence of new recurrences after the resection of the scar tissue. In our series, 5 out of the 22 patients had inflammatory diseases: one patient with amyloidosis, 3 with Wegener's granulomatosis and one with microscopic polyangiitis. In these patients, the endoscopic treatment improved the symptoms locally, at least temporarily. Nevertheless, the disease-free time was less than that of other tracheobronchial stenoses. From our standpoint, these are systemic diseases and we are merely intervening locally; therefore, the treatment of the underlying disease is of vital importance in these patients. In the case of Wegener's granulomatosis, treatment has been recommended with a combination of azathioprine and corticosteroids with the aim of minimizing the manipulation of the airways during the episodes of activity of this systemic disease.24–26 As for patients with amyloidosis, the lack of success in the treatment is probably due to the frequent bleeding that is produced in this disease because of the increase in the friability of the artery walls. In these patients, it is preferable to use instruments with a deeper coagulation effect, like ND-YAG laser.
The results obtained in this study enable us to recommend the use of endobronchial scalpels in all the bronchoscopy units in Spain, in combination with the Endo-cut I (ERBE) cut mode available on the VIO generator (ERBE, Germany). This technique allows for urgent solutions in cases of tracheal stenoses that put the lives of patients at risk, especially those in whom tracheostomy would not be a solution. It would be indicated for short web-like stenoses of the airway while a more complete treatment is scheduled, which could be a surgical treatment or a complete endoscopic treatment. The completed endoscopic treatment should be complemented with mechanical balloon dilation or rigid bronchoscopy. In addition, in recent years, it has been proposed to use topical triamcinolone with the help of a transbronchial needle that could contribute to avoiding re-stenosis. In addition, Cosano-Povedano have published an article about the efficiency of mitomycin C after recanalization with electrocautery and balloon dilatation with the aim to avoid re-stenosis in patients with lung trasplantation.27–31 Both treatments can be considered in patients with recurring stenosis after having performed recanalization with the endobronchial scalpel in combination with the dilation balloon and/or the bezel of the rigid bronchoscope.
In conclusion, and based on the Latin expression primum non nocere, the use of this new intermittent and optimized cutting mode, Endo-cut I, in combination with the endobronchial scalpel and the isolated-tip scalpel, is a safe and effective treatment in the case of patients with web-like tracheobronchial benign stenoses. This technique produces clinical and functional improvement in all patients, requiring a second intervention in less than half of the patients. In comparison with ND-YAG laser, it causes less fibrin plates. This is probably because the cuts done with the endobronchial scalpel are thinner and because the Endo-cut I presents a smaller coagulating effect as the power emitted by said cutting program adjusts to the resistance of the tissue. This breaks the vicious circle of scarring and re-stenosis, which at the same time leads to a greater disease-free interval and, in certain cases, such as in radiogenic scars, to a cure.
Conflict of InterestsThe authors declare having no conflict of interests.
The authors would like to thank all of the collaborators, especially the endoscopy and lung function testing staff, for their participation in this study. We would also like to thank the ERS and ELF for granting Beatriz Amat an ERS fellowship, and also Dr. Martín, Dr. García Pachón and Dr. Freitag for their support. Thanks to my tutor Dr. Reichle for teaching me about medicine and about life. In memoriam Dr. Med. Hans-Jürgen Rohde.
Please cite this article as: Amat B, et al. Tratamiento endoscópico de las estenosis benignas traqueobronquiales tipo web-like con el bisturí endobronquial en combinación con un programa de corte optimizado. Arch Bronconeumol. 2011;48:14–21.
Beatriz Amat is the recipient of the ERS/ELF fellowship number 62.