Road traffic accidents are one of the main causes of death worldwide and are clearly associated with sleepiness. Individuals with undiagnosed sleep apnea–hypopnea syndrome (SAHS) are among the population with a high risk of experiencing sleepiness at the wheel and, consequently, road traffic accidents. Treatment with continuous positive airway pressure (CPAP) has been shown to reduce the risk of accidents among drivers with SAHS. For this reason, the European Union has included this disease in the psychological and physical criteria for obtaining or renewing a driving license. To comply with this European Directive, Spain has updated its driving laws accordingly. To facilitate the implementation of the new regulations, a group of experts from various medical societies and institutions has prepared these guidelines that include questionnaires to screen for SAHS, diagnostic and therapeutic criteria, and physician's report templates.
Los accidentes de tráfico son una de las principales causas de mortalidad en todo el mundo, y la somnolencia está claramente relacionada con ello. Entre la población con alto riesgo de padecer somnolencia al volante, y consecuentemente accidentes de tráfico, se encuentran las personas que tienen síndrome de apnea del sueño (SAHS) sin diagnosticar. El tratamiento con CPAP ha demostrado una disminución en el riesgo de accidentabilidad de conductores con SAHS. Es por ello que la Unión Europea ha incluido esta enfermedad entre los requisitos psicofísicos para obtener o mantener el permiso de conducción. Para cumplir con esta Directiva Europea, España ha actualizado el Reglamento de Conductores de manera acorde. Con el fin de facilitar la implementación de la nueva norma, un grupo de expertos de diferentes sociedades médicas e instituciones han elaborado la presente guía, que contiene cuestionarios de cribado de SAHS, criterios de diagnóstico y tratamiento y modelos estandarizados de informes a completar por los médicos.
Traffic accidents are one of the major worldwide causes of death among individuals aged between 5 and 50 years. The death rate on the roads in the European Union (EU) is 52 deaths per million inhabitants, and in economic terms have been estimated to account for 1%–3% of the GDP of the respective countries, representing up to 500 billion dollars on a worldwide level.1
There is clear evidence that sleepiness, irrespective of its cause, is a significant risk factor for traffic accidents, although it is difficult to determine the exact figures. The National Highway Traffic Safety Administration calculates that 2.5% of fatal accidents and 2% of non-fatal accidents are related to sleepiness, although these numbers may be underestimated.2
Sagaspe et al.3 conducted a telephone survey among 4774 drivers, and found that 5.8% of the respondents had had an accident, 3.2% of which were related to sleepiness.
In a Spanish study of 4002 vehicle drivers, 3.6% regularly experienced sleepiness when driving; of these, 81% had fallen asleep at the wheel at some time, and 25% regularly did so. One of the main causes of habitual sleepiness while driving was sleep apnea.4
Goncalves et al.5 also provided interesting data associated with the prevalence of sleepiness and driving in Europe: in 12434 questionnaires completed in 19 EU countries, the mean prevalence of “falling asleep at the wheel in the last 2 years” was 17%, and of these, the median accident rate was 7% (3.2% of which were fatal).
Sleepiness among professional drivers is a particularly sensitive issue, in view of the possible consequences.6
The population at high risk of experiencing sleepiness at the wheel includes not only professional drivers, due to their longer times of exposure, but also people who work very long shifts or who drive at night, individuals who drive in a state of sleep deprivation, especially young people, or who sleep less than 6h, patients taking hypnotic drugs or other sleep-inducing medications, and finally, individuals with symptoms associated with undiagnosed sleep apnea.7
Various diseases, such as diabetes mellitus, cardiovascular diseases, psychiatric and neurological diseases, obesity or impaired vision, are associated with a higher incidence of traffic accidents,8 but sleep apnea–hypopnea syndrome (SAHS) is the disorder that most frequently causes sleepiness and an increased risk of accidents. Poor sleep hygiene must be added to this group of diseases.
A systematic review and metaanalysis9 of the risk of accidents among drivers of commercial vehicles published in 2009 showed that the mean risk was in the range of 1.21–4.89, and that the predictive factors for accidents among drivers with SAHS include body mass index (BMI), apnea–hypopnea index (AHI), oxygen saturation, and possibly daytime sleepiness. Young et al.10 showed that individuals with an AHI>5 were significantly more likely to have at least 1 accident in a 5-year period, and that men and women with AHI>15 had significantly more multiple accidents in the same period (odds ratio: 7.3).
Although the published studies differ, most of the evidence suggests that the risk of traffic accidents and sleep apnea is related more closely with sleepiness than with disease severity measured by AHI. The significance of sleepiness as a primary factor contributing to traffic accidents was recently supported by Karimi et al.11 who found that excessive daytime sleepiness (Epworth scale>15) is significantly associated with accident rates. Other studies, meanwhile, such as those of Terán-Santos et al.12 and the European Sleep Apnea Database (ESADA), associate AHI with accident rates.13
Several studies have evaluated the effect of continuous positive airway pressure (CPAP) on reducing motor vehicle accident rates in patients with SAHS, and in most studies, effective treatment will result in a substantial reduction or even normalization of the accident rate.14
The fact that untreated SAHS patients have a higher risk of traffic accidents has prompted some countries in the EU, including Spain, to list this disease among those that must be controlled before a driving license can be obtained or renewed. More recently, the EU Commission Driving License Directive 2014/85,15 modifying Directive 126/2006, has included SAHS among the criteria that appear in Annex III on the criteria for psychophysical aptitudes that must be evaluated in all Member States. This regulation was published in the EU in June 2014 and sets down the minimum criteria that must be applied in all countries.
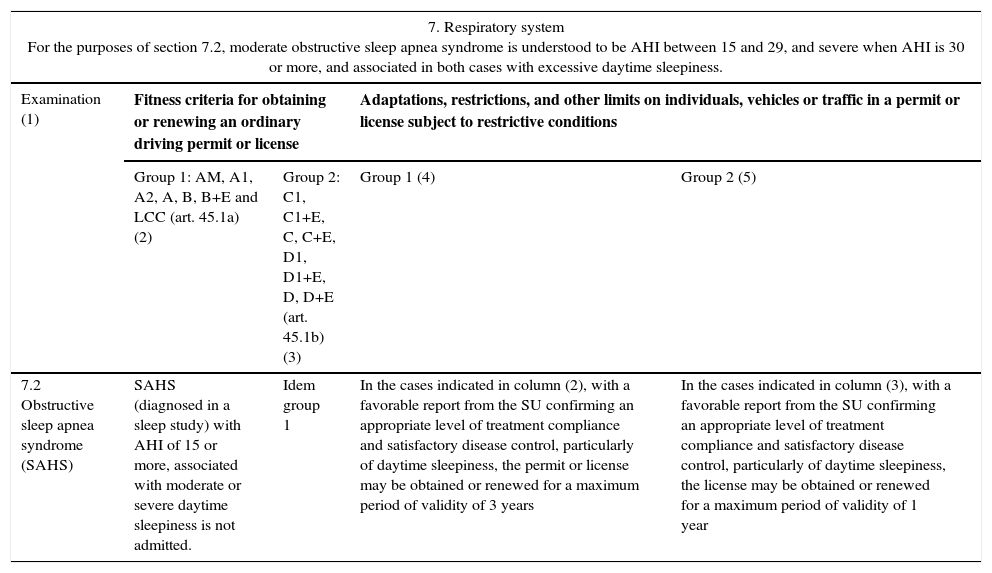
Spain, which already included SAHS in the General Regulations for Drivers, specifically in Annex IV, specifying criteria for psychophysical fitness for obtaining or renewing a driver's license, has updated their criteria in accordance with the European Directive with Royal Decree (RD) 1055/2015, 20 November 2015, modifying the General Regulations for Drivers approved by Royal Decree 818/2009, 8 May 2009, that became effective in January 2016 (Table 1). The annex regarding obtaining or renewing a driving license now includes criteria for moderate (AHI 15–29) and severe (AHI>30) SAHS, both associated with excessive sleepiness, and establishes that individuals with SAHS (diagnosed in a Sleep Unit [SU]) with an AHI of 15 or more associated with sleepiness cannot obtain or renew their driving license, unless they submit a favorable report from the SU stating that they comply appropriately with treatment and that their disease is clinically controlled to a satisfactory degree, particularly with regard to sleepiness. The period of validity of these licenses is limited to 3 years for group 1, and up to 1 year for group 2.
Content of Annex IV of the General Regulations for Drivers Approved by Royal Decree 818/2009, modified by RD 1055/2015 (Adapted from the Official State Bulletin).
| 7. Respiratory system For the purposes of section 7.2, moderate obstructive sleep apnea syndrome is understood to be AHI between 15 and 29, and severe when AHI is 30 or more, and associated in both cases with excessive daytime sleepiness. | ||||
|---|---|---|---|---|
| Examination (1) | Fitness criteria for obtaining or renewing an ordinary driving permit or license | Adaptations, restrictions, and other limits on individuals, vehicles or traffic in a permit or license subject to restrictive conditions | ||
| Group 1: AM, A1, A2, A, B, B+E and LCC (art. 45.1a) (2) | Group 2: C1, C1+E, C, C+E, D1, D1+E, D, D+E (art. 45.1b) (3) | Group 1 (4) | Group 2 (5) | |
| 7.2 Obstructive sleep apnea syndrome (SAHS) | SAHS (diagnosed in a sleep study) with AHI of 15 or more, associated with moderate or severe daytime sleepiness is not admitted. | Idem group 1 | In the cases indicated in column (2), with a favorable report from the SU confirming an appropriate level of treatment compliance and satisfactory disease control, particularly of daytime sleepiness, the permit or license may be obtained or renewed for a maximum period of validity of 3 years | In the cases indicated in column (3), with a favorable report from the SU confirming an appropriate level of treatment compliance and satisfactory disease control, particularly of daytime sleepiness, the license may be obtained or renewed for a maximum period of validity of 1 year |
AHI: apnea–hypopnea index; SU: sleep unit.
Studies in SAHS and driving show that the risk of a traffic accident in subjects with a diagnosis of SAHS depends not only on the diagnosis of the disease, but also on the different parameters that are also associated with a greater driving risk, and which might affect an individual's fitness to drive.13 This requires a personalized evaluation of the driver in Driving Examination Centers (DACs) and, consequently, the medical staff of these centers must be fully apprised of the impact of the disease on the subject before issuing the psychophysical fitness report.
Annex IV of the General Regulations for Drivers, RD 818/2009, modified by RD 1055/2015, states that to obtain or renew a driving license, drivers with a diagnosis of SAHS must provide the DAC with a report from an SU, which is taken into account in the definitive report on the individual's fitness to drive. The aim of the SU report is to inform the DAC physician of the diagnostic details, clinical manifestations of the disease (primarily sleepiness), and efficacy of treatment, so that the impact of the disease on driving can be evaluated and a report on the fitness of the subject to drive issued. Both the patient and doctors working in SUs must be aware of the need to present this report to the DAC at the time of either obtaining or renewing a driving license, since failure to present the report at the time of license renewal will lead to suspension of the process until such time as it is presented, with the consequent personal and professional inconveniences that such a situation may cause the driver.
Individuals who need to renew their driving license may face difficulties and variable access to SUs, depending on their healthcare areas, our group recommends that a standardized report template is issued for the purposes of obtaining and renewing a license, and that the patient is informed of the importance of such a report and their obligation to present it to the DAC. This report should be valid for a period of 6 months, unless the DAC detects any changes when administering their standard questionnaire.
Specific Recommendations for the Evaluation of Psychophysical Fitness to Drive Motor Vehicles in Patients With Sleep Apnea SyndromeDuring the course of their work, the DAC sees 2 large groups of drivers: those with a diagnosis of SAHS, and those without, but who, after clinical screening, are found to meet the established criteria for a high diagnostic suspicion of SAHS.
Drivers Diagnosed With Sleep Apnea–Hypopnea Syndrome in a Sleep UnitProposed recommendations for evaluating fitness to drive motor vehicles in patients with a diagnosis of SAHS are given below.
Fit to Drive- 1.
Patients with AHI<15 and/or without excessive sleepiness (Epworth<15), not receiving treatment.
- 2.
Patients with AHI>15<30 without excessive sleepiness (Epworth<15), not requiring treatment.
In patients in either group (1 and 2) who do not have sleepiness, whether AHI is higher or lower than 15, there is no absolute evidence of a greater risk of having a traffic accident, so they may be considered fit to drive, with no type of restriction. If, as a result of the diagnostic process, the patient is undergoing regular follow-up in the SU, they must provide follow-up reports when renewing their license with the normal expiry periods, stating that their situation remains unchanged. In these cases, the report may also be issued by the primary care physician, according to the clinical report from the SU.
- 3.
Drivers with no suspicion of SAHS after screening (see criteria in the following sections).
- 1.
Patients with AHI>15 with excessive sleepiness, receiving continuous positive airway pressure (CPAP) treatment.
A driver diagnosed with an AHI>15 in a sleep study, who also experiences sleepiness, must provide an SU report to the DAC for the purpose of evaluating their fitness to drive for both group 1 and group 2 licenses.
Patients receiving treatment with CPAP must use this report as proof that they are complying appropriately with their treatment, which in the case of CPAP treatment involves at least 4h/night for more than 70% of the week, and that excessive sleepiness has been controlled.
The driver who meets these conditions is considered fit to drive, with a reduced period of validity of their license (maximum 3 years for group 1, and 1 year for group 2). Reduction of the period of validity is the mechanism established in Annex IV of the General Regulations for Drivers to ensure that the patient is controlled.
- 2.
Patients with AHI>15 plus excessive sleepiness, receiving treatment other than CPAP: mandibular advancement device, surgery, weight loss, etc.
The SU report must confirm reduction of AHI<10 and control of sleepiness.
As before, the driver will be considered fit to drive, with a reduced period of validity of their license: maximum 3 years for group 1, and 1 year for group 2.
Patients with AHI>15 plus sleepiness who do not comply appropriately with treatment (irrespective of the type of treatment) and/or with uncontrolled symptoms.
For patients who are not fit to drive, either due to lack of treatment compliance or recently initiated treatment making it impossible to prove efficacy, a report of fit to drive with reduced period of validity may be issued in the following cases, provided an SU report is available:
- •
A driver whose treatment has been successful after a period of 4–6 weeks, with appropriate compliance and control of clinical symptoms. A reduced period of license validity of 1 year followed by evaluation of clinical stability may be established at the criteria of the physician, depending on the time of treatment and the patient's progress.
SU considerations:
- •
CPAP adjustments or mandibular advancement devices for treating SAHS in all cases must be regulated with self-adjusting systems or manual polysomnography titration.
- •
It is always recommended that these procedures are performed in SUs or by specialist physicians qualified in the study and treatment of sleep-disordered breathing.
- •
In some cases, depending on the criteria of specialists qualified in the study and treatment of sleep-disordered breathing, some objective measurements of sleepiness may be necessary (maintenance of wakefulness test, multiple sleep latency test, or OSLER test).
- •
For group 2 drivers, a sleep study with adjustment of treatment to reduce AHI to figures lower than 10 and control excessive sleepiness is recommended.
In view of the scientifically proven relationship between sleep apnea and traffic accidents, it is recommended that drivers without a diagnosis be screened for the presence of SAHS.
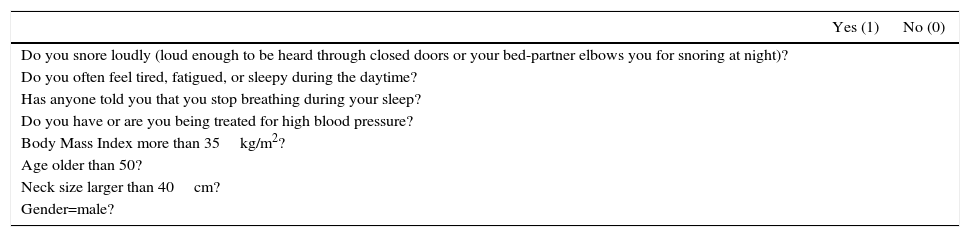
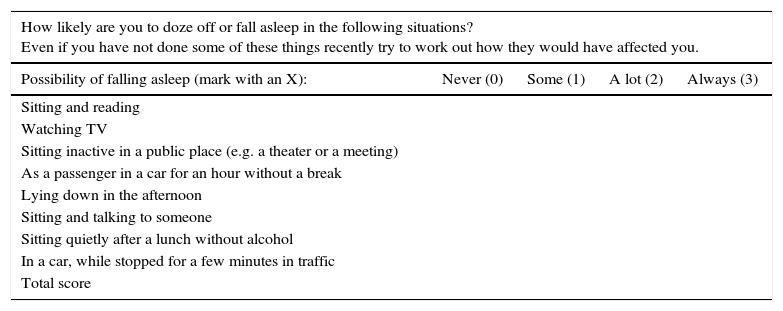
The chosen screening method is the STOP-Bang questionnaire, given its high sensitivity and ease of application in all settings (Table 2), in combination with the Epworth Sleepiness Scale (Table 3), and history of traffic accidents with victims associated with excessive sleepiness when driving in the past 3 years.16–19
STOP-Bang Questionnaire.
| Yes (1) | No (0) | |
|---|---|---|
| Do you snore loudly (loud enough to be heard through closed doors or your bed-partner elbows you for snoring at night)? | ||
| Do you often feel tired, fatigued, or sleepy during the daytime? | ||
| Has anyone told you that you stop breathing during your sleep? | ||
| Do you have or are you being treated for high blood pressure? | ||
| Body Mass Index more than 35kg/m2? | ||
| Age older than 50? | ||
| Neck size larger than 40cm? | ||
| Gender=male? |
Final score: low (<2); intermediate (3–4); high (>5).
Epworth Sleepiness Scale.
| How likely are you to doze off or fall asleep in the following situations? Even if you have not done some of these things recently try to work out how they would have affected you. | ||||
|---|---|---|---|---|
| Possibility of falling asleep (mark with an X): | Never (0) | Some (1) | A lot (2) | Always (3) |
| Sitting and reading | ||||
| Watching TV | ||||
| Sitting inactive in a public place (e.g. a theater or a meeting) | ||||
| As a passenger in a car for an hour without a break | ||||
| Lying down in the afternoon | ||||
| Sitting and talking to someone | ||||
| Sitting quietly after a lunch without alcohol | ||||
| In a car, while stopped for a few minutes in traffic | ||||
| Total score | ||||
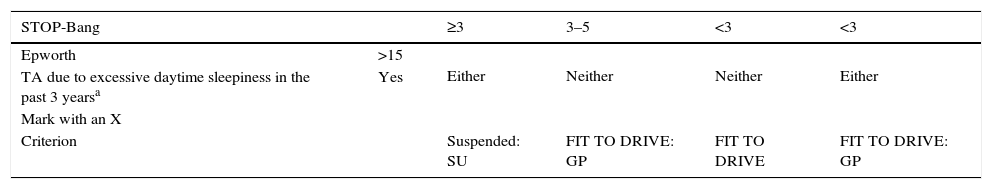
The following steps will be taken, depending on the scores obtained in these questionnaires (Table 4):
- •
If the person who completes the questionnaire has a STOP-Bang score≥3 and/or has any of the 2 associated criteria (Epworth Sleepiness Scale>15 or a traffic accident with consequences due to sleepiness in the past 3 years), their license will be suspended and they must be referred for an SU study, given their high probability of having moderate/severe SAHS, using the proposed form (Table 5). If applicable, the SU will perform a diagnostic and therapeutic study within 1 month.
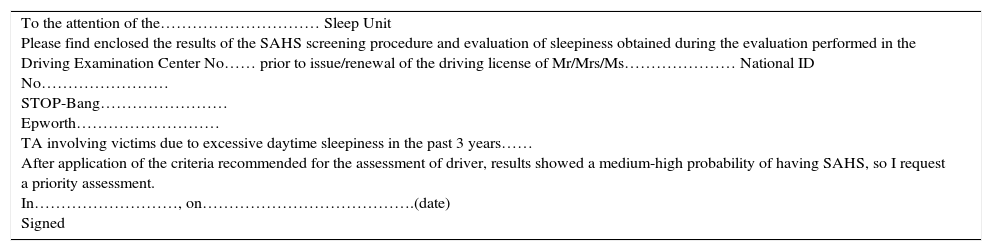
Table 5.Proposed Report to be Issued by the Driver Assessment Centers for Referral to the Sleep Unit of Drivers With Suspected SAHS. Driver Code.
To the attention of the………………………… Sleep Unit
Please find enclosed the results of the SAHS screening procedure and evaluation of sleepiness obtained during the evaluation performed in the Driving Examination Center No…… prior to issue/renewal of the driving license of Mr/Mrs/Ms………………… National ID No……………………
STOP-Bang……………………
Epworth………………………
TA involving victims due to excessive daytime sleepiness in the past 3 years……
After application of the criteria recommended for the assessment of driver, results showed a medium-high probability of having SAHS, so I request a priority assessment.
In………………………, on………………………………….(date)
Signed - •
If the STOP-Bang questionnaire score is between 3 and 5 and the additional criteria are negative, the subject may be considered fit to drive and referred to their primary care physician for evaluation.
- •
If the STOP-Bang questionnaire score is <3 points and the additional criteria are negative, the subject is considered fit to drive.
- •
If the STOP-Bang questionnaire score is <3 but the subject presents either of the additional criteria, they may be considered fit to drive and must be referred to their primary care physician for evaluation.
Screening Criteria According to Questionnaire Results.
| STOP-Bang | ≥3 | 3–5 | <3 | <3 | |
|---|---|---|---|---|---|
| Epworth | >15 | Either | Neither | Neither | Either |
| TA due to excessive daytime sleepiness in the past 3 yearsa | Yes | ||||
| Mark with an X | |||||
| Criterion | Suspended: SU | FIT TO DRIVE: GP | FIT TO DRIVE | FIT TO DRIVE: GP | |
TA: traffic accidents; Epworth: Epworth sleepiness scale; GP: general practitioner; SU: Sleep Unit.
The driver must sign the clinical history to attest to the accuracy of the report.
A suspicion of SAHS after screening puts the DAC doctor in the delicate position of weighing up the rights of the individual against their personal risk and risk to others. The skill of the SU in managing the study of these patients is essential from a preventive perspective.
Content of the Sleep Unit Report Providing Supportive Data to the Driver Assessment CenterThe report from the SU, in accordance with the provisions of Annex iv of the General Regulations for Drivers must cover the following:
- -
AHI at the time of diagnosis, and the presence or absence of sleepiness and severity (mild, moderate, severe).
- -
Type of treatment and if therapeutic compliance is adequate (see criteria below).
- -
Appropriate control of the disease, including control of sleepiness.
When the report is given to the patient in the SU, the patient should sign it along with the physician, indicating that they have been appropriately informed and are in agreement with the content of the report.
It is recommended that the SU and specialist physicians qualified in the study and treatment of sleep-disordered breathing issue a clinical report stating the level of compliance and clinical control of symptoms. We do not advise SU professionals to include their opinion on the ability of the SAHS patient to drive. Coexistence of other diseases/circumstances might affect the final report issued by the DAC, and a statement in the SU report could cause conflicts between the driver and the DAC professionals.
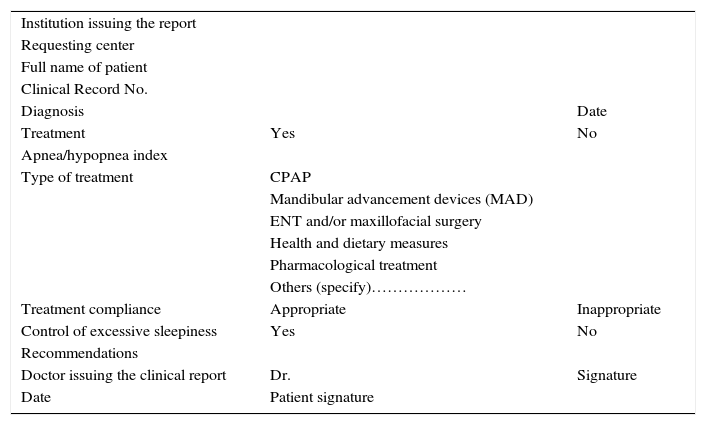
A standard report template (Table 6) is proposed, to which general criteria on sleep habits and specific criteria on sleep and driving (additional material) will be attached. These messages will support the health advice that will also be provided in the DAC setting.
Proposed Report to be Issued by Sleep Units to Driver Assessment Centers on the Clinical Status of the Patient's Sleep Disorder (Applicable to SAHS and Other Sleep Disorders).
| Institution issuing the report | ||
| Requesting center | ||
| Full name of patient | ||
| Clinical Record No. | ||
| Diagnosis | Date | |
| Treatment | Yes | No |
| Apnea/hypopnea index | ||
| Type of treatment | CPAP | |
| Mandibular advancement devices (MAD) | ||
| ENT and/or maxillofacial surgery | ||
| Health and dietary measures | ||
| Pharmacological treatment | ||
| Others (specify)……………… | ||
| Treatment compliance | Appropriate | Inappropriate |
| Control of excessive sleepiness | Yes | No |
| Recommendations | ||
| Doctor issuing the clinical report | Dr. | Signature |
| Date | Patient signature |
Adapted from the National Consensus on sleep apnea–hypopnea syndrome. Spanish Sleep Group 2005.
- •
This questionnaire template should ideally be included in hospital clinical records.
- •
It will be disseminated via the websites of the scientific societies involved in the diagnosis and treatment of SAHS, thus promoting the use of this standard report.
The DAC will also provide a copy to patients with suspected SAHS for completion by the SU physician after the sleep study.
ConclusionsExcessive sleepiness affects 5%–20% of the population. This problem, together with fatigue, increases the risk of traffic accidents. In total, 3.6% of drivers habitually experience sleepiness while driving.
SAHS is the treatable medical condition most commonly associated with traffic accidents caused by sleepiness.
There is an individual relationship between hours slept and the development of excessive daytime sleepiness.
The population at high risk of experiencing sleepiness at the wheel includes not only professional drivers who have longer times of exposure, but also people who work very long shifts, individuals who drive in a state of sleep deprivation, especially young people, or who sleep less than 6h, patients who use alcohol, hypnotic drugs or other medications that can cause sleepiness, and finally, individuals with symptoms associated with undiagnosed sleep apnea or other sleep disorders.
Every effort should be made to raise awareness of the importance of respecting rest times among professional drivers, so that work interests do not put the safety of drivers or other road users at risk.
Treatment of patients with sleep apneas reduces the number of accidents and associated costs.
Final ConsiderationThe editorial team of these guidelines on procedures in sleep apnea and driving states that the content of this paper is based on current levels of scientific knowledge and that the rate of accidents caused by sleep apneas depends on multiple variables associated with the presence of comorbidities and lifestyle, among other factors.
Conflict of InterestsThe authors state that they have no conflict of interests.
Participating Societies and InstitutionsSpanish Sleep Society (SES).
Spanish Society of Pulmonology and Thoracic Surgery (SEPAR).
Instituto Carlos III, CIBEReS.
Spanish Traffic Medicine Society.
Spanish Ministry of Health, Social Services and Equality.
General Subdepartment of Road Policies, General Department of Traffic.
Our thanks to Blanca Barriuso Esteban (edition of text format), Sleep Unit, Hospital Universitario de Burgos.
Please cite this article as: Terán-Santos J, Egea Santaolalla C, Montserrat JM, Masa Jiménez F, Librada Escribano MV, Mirabet E, et al. Apnea del sueño y conducción de vehículos. Recomendaciones para la interpretación del nuevo Reglamento General de Conductores en España. Arch Bronconeumol. 2017;53:336–341.