Shrinking lung syndrome (SLS) is a rare complication of Sjögren's syndrome. We report the case of a woman diagnosed 5 years previously with primary Sjögren's syndrome (pSS) who presented SLS. She received steroids, azathioprine and cyclophosphamide, with no response, yet showed remarkable clinical and functional improvement after starting treatment with rituximab.
A 47-year-old woman, with a 5-year diagnosis of pSS, was hospitalized for an 8-week history of left pleuritic pain, discomfort in both sides of the chest and dyspnea on medium effort. Initially, she had been given a presumed diagnosis of right lower lobe pneumonia, but did not respond to treatment. On examination, her breathing rate was 22 breaths/minute, and reduced breath sounds were detected in the right lung base. Chest X-ray showed loss of volume in the right hemithorax and computed tomography angiography revealed areas of atelectasis in the right basal subsegment, right hemidiaphragm elevation, minimal left pleural thickening, and no evidence of pulmonary embolism. Lung function tests showed a severe restrictive pattern. Fiberoptic bronchoscopy was performed and no changes were observed. Electromyography of the phrenic nerve showed signs of partial axonotmesis.
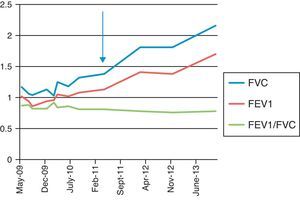
SLS was diagnosed and the dose of prednisone was increased to 45mg/day. Inhaled salbutamol and theophylline were added, but dyspnea and lung function failed to improve after 3 months of treatment. In view of this lack of response, azathioprine and later cyclophosphamide were added, but no clinical or functional response was observed. We then decided to try i.v. administration of anti-CD20 monoclonal antibody (rituximab) 1g repeated after 2 weeks. Clinical, radiological and functional improvement was achieved (Fig. 1), and the patient remained asymptomatic 2 years later.
Shrinking lung syndrome (SLS) is a complication that has been described in some (0.9%) patients with systemic lupus erythematosus (SLE).1 It is, however, exceptional in other autoimmune diseases.2 It most commonly presents with dyspnea, persistent episodes of chest pain, progressive loss of lung volume, and absence of significant interstitial and/or pleural disease on computed tomography.1 Its pathogenesis is still a source of controversy, and many hypotheses have been proposed.3 In 1965, Hoffbrand and Beck suggested that microatelectasis and hyaline membranes caused by surfactant deficiency may be involved. Other authors considered SLS to be a form of diaphragmatic myopathy and phrenic nerve neuropathy, but none of these theories could be demonstrated in subsequent studies.3 In our patient, changes in the electromyography consistent with partial axonotmesis were found, and we concluded that right phrenic neuropathy was the probable causative mechanism. Treatment with corticosteroids can reduce symptoms and improve lung function, but other treatments have provided benefit in some patients, including theophylline and immunosuppressive agents, such as cyclophosphamide and azathioprine.1–3 Three cases of good therapeutic response to rituximab have been reported, all in SLE patients.4,5 Although SLS can be successfully treated with steroids, salbutamol and theophylline in most cases, it can be a source of significant morbidity and occasionally mortality – in one report, it was impossible to wean the patient from the ventilator.3
In conclusion, our case supports the use of rituximab in patients with pSS-related SLS, refractory to steroids and immunosuppressive drugs, although the exact mechanism behind the improvement seen with B cell depletion remains unclear.
Conflict of InterestsThe authors declare that they have conflict of interests.
Please cite this article as: Blanco Pérez JJ, Pérez González A, Guerra Vales JL, Melero Gonzalez R, Pego Reigosa JM. Síndrome del pulmón encogido en el síndrome de Sjögren primario tratado con éxito con rituximab. Arch Bronconeumol. 2015;51:475–476.