The latest version of the Spanish Chronic Obstructive Pulmonary Disease Guidelines (GesEPOC), published in 2017, stratifies patients into 2 risk groups (low and high) according to 3 criteria: lung function, degree of dyspnea, and history of exacerbations.1 This stratification is the cornerstone for guiding the intensity of drug treatment. In contrast to the GesEPOC, the latest versions of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) document propose pharmacological therapeutic algorithms based on the classification of risk into 4 groups (ABCD). Unlike earlier versions, they do not use lung function for classification, although it is clearly pointed out that this variable predicts mortality and serves to guide non-pharmacological treatments, so it is assessed independently on a numerical scale (1–4).2 Removing the criterion of lung function from the “ABCD” classification means that some subjects previously classified in high-risk groups are now reclassified as low risk, possibly leading to therapeutic changes, which generally involves a reduction in the intensity of drug treatment. This a move that has generated some debate,3,4 and it raises the question whether the decision of the GesEPOC to include lung function as an integral part of risk stratification is appropriate and adds value with respect to the other 2 criteria (dyspnea and exacerbations), since the GesEPOC risk groups have not yet been validated.
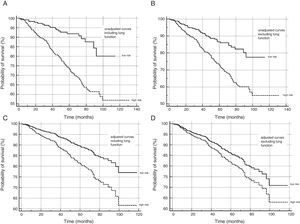
Consequently, we designed this study with the intention of delving deeper into this issue. We retrospectively reviewed patients seen in the dedicated COPD clinic of a second level university hospital. The study population comprised all consecutive patients with a diagnosis of COPD according to the GOLD initiative criteria2 attending this clinic between January 2008 and April 2018 (976 subjects). The participants were selected from a healthcare database containing systematic records of patient data, such as lung function, history of moderate and severe exacerbations the year prior to the date of the first assessment in the clinic, and degree of dyspnea (mMRC). GesEPOC risk criteria were available for all patients. Two quantitative scales were developed on the basis of the number of risk factors present in each case using 2 methods: (1) including all GesEPOC criteria (score: 0–3), and (2) excluding the FEV1 criterion (score: 0–2). We tested the ability of these 2 quantitative scales to predict overall mortality using receiver-operator curves, comparing their areas according to the method of DeLong et al.5 Each subject was then classified as high or low risk (1) in accordance with GesEPOC-2017 and (2) without considering lung function, and survival curves were obtained for the risk groups defined using both methods, unadjusted using the Kaplan–Meier method, and adjusted for the covariates age, sex, comorbidity (Charlson index), pack-year index, and body mass index, using Cox proportional hazards model analysis.
Patients were excluded as follows: 41 patients who had a follow-up of less than 6 months, 7 who had undergone lung transplantation, and 8 who were lost to follow-up. Study population: 920 subjects; age: 69.3±9.5 years; men: 730 (79.3%); average FEV1%: 51.5±16.8; average SpO2: 93.3±4.4%; patients with SpO2<90%: 139 (15.1%). A total of 677 (73.5%) cases were classified as high risk according to GesEPOC. When the lung function criterion was excluded, 559 (60.7%) patients were high risk. Mean follow-up time was 55.6±27.4 years. There were 217 deaths (23.5%) within a mean of 39.3±23.1 months after the first visit.
The area under the receiver-operator curve to predict mortality for the quantitative scale, which included all the GesEPOC criteria, was 0.70 (IC 95% 0.67–0.73), which was significantly higher than for the scale that excluded lung function: 0.67 (95% CI 0.64–0.70) (difference: 0.03, 95% CI 0.01–0.05, P=0.0007). Fig. 1 shows the survival curves, unadjusted and adjusted for confounding variables, for patients at high and low risk, including and excluding the lung function criterion. High and low-risk patients showed differences in survival in all cases, the major differences being observed when the lung function criterion was included.
Our study shows that the GesEPOC risk stratification is appropriate, and that including lung function is useful for predicting mortality, compared to a classification that excludes this variable. Due to the limitations of the study design, we cannot determine if lung function also provides added value to the other 2 parameters in the prediction of other clinical outcomes, such as the incidence of future exacerbations. This is an important limitation, since the main objective of the risk group classification is to guide treatment, and it has not yet been demonstrated whether guiding treatment on the basis of this risk classification impacts on clinically relevant outcomes and, in particular, whether the inclusion of lung function in the decision to intensify the therapies has any effect on mortality.
Our study has some limitations: it is retrospective, although the parameters were collected systematically in a healthcare database, so very few variables were unavailable. In this regard, clinical histories in our setting are fully computerized, so reliable data could be obtained on the outcome variable (all-cause mortality). The analysis would require external validation, as it was carried out in a single center which, moreover, it was a dedicated clinic, implying selection bias, as confirmed by the high percentage of high-risk cases included. Furthermore, the follow-up period is long and the possible variations in the treatments over time or their influence on mortality could not be assessed.
Despite these drawbacks, we believe that the study supports the validity of the GesEPOC risk stratification strategy, and that this could be a point of departure for future well designed studies exploring the effect on clinical outcomes of guiding treatment on the basis of this classification.
Please cite this article as: Golpe R, Suárez-Valor M, Veiga-Teijeiro I, Veres-Racamonde A, Pérez-de-Llano LA. ¿Debe incluirse la función pulmonar en la estratificación de riesgo de la enfermedad pulmonar obstructiva crónica propuesta por GesEPOC? Arch Bronconeumol. 2019;55:436–437.