Cystatin C is an endogenous protease inhibitor that can be detected in serum and in biological fluids. Its main clinical utility is as a marker in the study of impaired renal function.1 However, it is known to have a role in the regulation of other diseases,2 and this has led to a growing interest in its determination in several different pathologies, including heart failure,3 cancer progression,4 immune disorders,5 and COPD prognosis.6
The presence of cystatin C has also been described in pleural fluid,7 and it has been suggested that it may be a useful diagnostic marker in the study of the etiology of pleural effusion.8 However, this possibility has not been assessed in any depth, and the results are limited to a small number of patients.
The aim of our study was to analyze cystatin C levels in pleural fluid, and explore their potential contribution to the diagnostic evaluation of effusions. For this purpose, we carried out a prospective study in consecutive patients with pleural effusion undergoing diagnostic thoracentesis. We collected the following data from each patient: age, sex, and biochemical analysis of pleural fluid and blood. Only the results obtained from the first thoracentesis were taken into account. The study was approved by the Clinical Research Ethics Committee of our hospital.
The study included 87 patients (42 women, 48%) with a mean (± SD) age of 70 (± 14) years. Effusions comprised 21 (24%) transudates and 66 exudates (76%). Of the exudates, 14 (21%) were of infectious origin, 21 (32%) were due to other benign processes (47%), and 31 were associated with malignant diseases. We analyzed the level of cystatin C in pleural fluid and the cystatin C/creatinine ratio to normalize values according to kidney function. Results were compared using analysis of variance, and the values of sensitivity, specificity, and goodness-of-fit were tested using the area under the receiving operating characteristic (ROC) curve. A P value <0.05 was considered statistically significant.
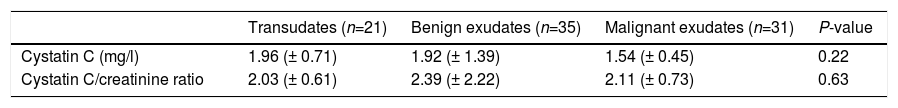
Table 1 shows the values of interest in the 3 groups (transudates, benign exudates, and malignant exudates). The differences between the different diagnostic groups did not reach statistical significance. The areas under the curve for differentiating transudates and exudates and for differentiating benign exudates from malignant exudates were, in all cases, lower than 0.70. Cut-off values for sensitivity and specificity that would improve the results described could not be established for the conventional criteria or routinely used parameters.9,10
Cystatin C values and the cystatin C/creatinine ratio.
| Transudates (n=21) | Benign exudates (n=35) | Malignant exudates (n=31) | P-value | |
|---|---|---|---|---|
| Cystatin C (mg/l) | 1.96 (± 0.71) | 1.92 (± 1.39) | 1.54 (± 0.45) | 0.22 |
| Cystatin C/creatinine ratio | 2.03 (± 0.61) | 2.39 (± 2.22) | 2.11 (± 0.73) | 0.63 |
Values shown as mean (± SD).
The determination of biochemical parameters in pleural fluid is a fundamental step in diagnostic studies and guides the initial diagnosis.9,11 In addition to the usual parameters for differentiating transudates from exudates, for diagnosing tuberculosis, or for determining the prognosis of parapneumonic effusions, some determinations have been shown to be of great use because they are characteristic of certain specific etiologies.10,12 The recent interest in cystatin C due to its role in various diseases and the initial description of cystatin C levels in pleural fluid justified a proper methodological assessment of its possible diagnostic utility. Domej et al. found that cystatin C values in pleural fluid could vary depending on the etiology of the effusion.8 In their pilot study, the authors obtained higher concentrations of cystatin C in pleural fluid in effusions of infectious origin. However, their findings were limited to a small number of patients. In our experience, cystatin C values in pleural fluid (direct or corrected according to renal function) did not differ significantly among the different diagnostic groups. In contrast to the findings of Domej et al.,8 we did not obtain results that might suggest that the determination of these parameters would be of potential use in clinical practice.
Please cite this article as: Soler-Sempere MJ, Pellicer-Mas M, Quevedo-Sánchez B, García-Pachón E. Cistatina C en el derrame pleural. Arch Bronconeumol. 2019;55:438.