We report the case of a 59-year-old man who presented in the emergency room with a 48-h history of fever 38.8°C, dyspnea and cough. He had a prior diagnosis of cryptogenic organizing pneumonia and was receiving prednisone 70mg/day and azathioprine 25mg/day.
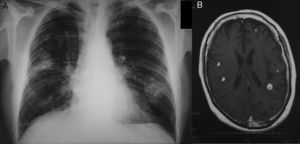
Physical examination showed fever 37.9°C, blood pressure 135/78mmHg, breathing rate 28 breaths/minute and heart rate 103 beats/minute, with bilateral fine crackles on lung auscultation. Blood test results showed 16600 leukocytes, 303000 platelets, and normal serum biochemistry (including liver function tests and procalcitonin), with the exception of C-reactive protein 5.7mg/dl. Baseline arterial blood gases were pO2 63mmHg, pCO2 36mmHg, pH 7.43 and oxyhemoglobin saturation 91%. Standard posteroanterior chest X-ray revealed cavitated alveolar infiltrate in the right upper lobe and infiltrate without cavitation in the left lower lobe (Fig. 1A).
Two blood cultures were performed, in aerobic and anaerobic media, and empirical treatment was started with piperacillin-tazobactam. Urine was negative for pneumococcal and Legionella antigens. After 4 days of antibiotic treatment without improvement, a chest–abdomen CT was performed, confirming previous radiological findings, with no other changes. Rhodococcus equi was isolated from both blood cultures, so based on susceptibility test results treatment was switched to imipenem, rifampicin and gentamicin. After 10 days of hospitalization, the patient began to complain of headache and instability, so magnetic resonance imaging (MRI) of the head was performed (Fig. 1B), revealing 8 cortical-subcortical nodular lesions, less than 1cm in size, indicative of brain abscesses.
Intravenous treatment was maintained for 2 months, followed by 4 more months of oral azithromycin and trimethoprim-sulfametoxazole. After 2 weeks of treatment, respiratory clinical signs had resolved and chest X-ray was normal. One month later, blood cultures were negative, and neurological signs had resolved. A follow-up head MRI at 3 months was normal.
There are more than 15 Rhodococcus species ubiquitous in the environment. They are strictly aerobic, intracellular Gram-positive coccobacilli that infect macrophages and polymorphonuclear cells. Some uncommon species, such as R. luteus, R. erythropolis, R. ruber and R. rhodochrous, mainly cause skin and corneal infections. R. equi, primarily transmitted via inhalation from contact with animals, is the most common and most pathogenic in humans. Cell immunosuppression is the major risk factor for infection, particularly in patients with acquired immunosuppression due to human immunodeficiency virus (HIV), although 10%–15% of infections occur in immunocompetent patients.1,2 The most common form of presentation in immunocompromised patients is cavitated pneumonia of the lower lobes3 (84%), while in immunocompetent patients, infections tend to be localized and extrapulmonary (42%),3,4 generally involving the central nervous system (abscesses, meningitis, etc.) and the skin (abscesses).
The respiratory process is insidious, manifesting as high fever, cough, dyspnea, chest pain and weight loss.2 It is identified and diagnosed from the culture of affected tissue samples.4 Blood cultures are positive in 50% of immunocompromised subjects, as was the case for our patient, and in 10% of immunocompetent subjects.5 There is no standard treatment. Rhodococcus is resistant to betalactams, except for imipenem, and susceptible to macrolides, rifampicin, aminoglycosides and vancomycin. Susceptibility to fluoroquinolones, clindamycin, trimethoprim-sulfamethoxazole and tetracyclines is variable.1,5 Treatment with 2 or 3 drugs is recommended, of which at least 1 should have good intracellular activity, such as rifamipicin or azithromycin.4,5
In immunocompetent subjects with localized infection, successful outcomes have been reported with a combination of 2 antibiotics for 2–8 weeks.2 Treatment can be extended for up to 6 months1 if the patient remains immunocompromised, and in cavitated pulmonary lesions or CNS involvement, as occurred in our case.
Mortality in immunocompetent patients is 11%, while in HIV patients it is 50%–55%, and 20%–25% in non-HIV-infected immunocompromised patients.2–4
Please cite this article as: Enríquez Rodríguez AI, García Clemente M, Buchelli Ramírez HL. Neumonía grave por Rhodococcus equi con diseminación hematógena al sistema nervioso central en un paciente inmunodeprimido. Arch Bronconeumol. 2015;51:203–204.