The use and combination of different central nervous system (CNS) depressants in elderly patients is a growing practice. This therapy is not without its complications, most notably respiratory center depression and respiratory acidosis requiring ventilatory support. It is therefore essential to be aware of these complications and identify which patients are at greater risk.
We present the findings from a series of patients admitted to the Respiratory Monitoring Unit of the Hospital Universitario de La Princesa (Madrid) over a period of 2 years. During this time, 302 patients were admitted with respiratory acidosis. A study of their medical records and urinalysis showed that in 10 cases (3.3%) the condition was associated with the use of CNS depressants. The doses given were estimated from clinical interview with the patient and/or carer, and in all cases drug-specific antagonists were used, together with non-invasive mechanical ventilation (NIV). Patients requiring emergency orotracheal intubation, patients transferred to the Intensive Care Unit for monitoring or intensive care, and those in whom NIV was ruled out by the Respiratory Medicine Department (approximately 12% of all patients admitted for respiratory acidosis) were excluded from the series. At admission, mean pH was 7.28 and mean PaCO2 was 69.4mmHg, both determined by arterial blood gas measurement. In many cases, progress was determined by other hypoventilation factors.
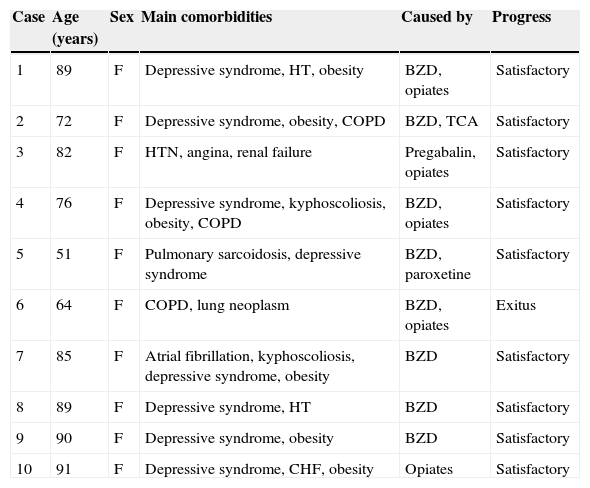
All patients included in the series were women with a mean age of 78.9 years. Of these, 80% were under treatment for a depressive syndrome, and 50% regularly took more than 2 CNS depressants. The combination drugs given were benzodiazepines (BZD), in 50%, and opiates, in 10%. This combination was responsible for 30% of cases. Predisposing factors, in addition to the therapy given, were found in 80% of patients (obesity in 60%, chronic obstructive pulmonary disease [COPD] in 30%, and kyphoscoliosis in 20%). In 1 case, drug toxicity was the result of an attempted suicide, and the patient died (Table 1).
Clinical Characteristics of the Sample.
| Case | Age (years) | Sex | Main comorbidities | Caused by | Progress |
|---|---|---|---|---|---|
| 1 | 89 | F | Depressive syndrome, HT, obesity | BZD, opiates | Satisfactory |
| 2 | 72 | F | Depressive syndrome, obesity, COPD | BZD, TCA | Satisfactory |
| 3 | 82 | F | HTN, angina, renal failure | Pregabalin, opiates | Satisfactory |
| 4 | 76 | F | Depressive syndrome, kyphoscoliosis, obesity, COPD | BZD, opiates | Satisfactory |
| 5 | 51 | F | Pulmonary sarcoidosis, depressive syndrome | BZD, paroxetine | Satisfactory |
| 6 | 64 | F | COPD, lung neoplasm | BZD, opiates | Exitus |
| 7 | 85 | F | Atrial fibrillation, kyphoscoliosis, depressive syndrome, obesity | BZD | Satisfactory |
| 8 | 89 | F | Depressive syndrome, HT | BZD | Satisfactory |
| 9 | 90 | F | Depressive syndrome, obesity | BZD | Satisfactory |
| 10 | 91 | F | Depressive syndrome, CHF, obesity | Opiates | Satisfactory |
BZD: benzodiazepines; CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; F: female; HTM: hypertension; TCA: tricyclic antidepressants.
BZDs are anxiolytic, hypnotic, anticonvulsant and antispasmodic drugs that enhance the inhibitory action of gamma-aminobutyric acid (GABA) receptors in the CNS. Opiates specifically bind to different central and peripheral receptors to regulate pain, amongst other actions. The use of these drugs, particularly in combination, inhibits the activity of the medullary and bulbopontine respiratory centers, which in turn diminishes the ventilatory response to hypoxia and hypercapnia, and can cause respiratory acidosis.1,2 This is particularly important in elderly patients with chronic pulmonary disease.3 Recent studies in patients with severe COPD have shown that high dose BZDs and opiates are associated with increased mortality.4 Long-term use of BZDs has also been associated with onset of acute hypercapnic respiratory failure in obese patients with sleep apnea/hypopnea syndrome (SAHS).5
In conclusion, patients with alveolar hypoventilation (SAHS, obesity, COPD) taking CNS depressants (BZD, opiates, etc.) alone or in combination are at greater risk of respiratory acidosis. It is important to bear this in mind when considering the use of these drugs in this high-risk population.
Please cite this article as: Alonso T, García E, Segrelles G, Zamora E. Acidosis respiratoria secundaria a fármacos. Arch Bronconeumol. 2015;51:204–205.