We describe a rare case of septic shock of pulmonary origin due to Rhodococcus equi, an emerging intracellular bacterium that causes zoonosis in our environment. Although generally transmitted to humans by inhalation, on this occasion contact with manure in an immunosuppressed patient with chronic myelomonocytic leukaemia (CMML) caused a serious lung infection.
Clinical CaseWe present the case of a 79-year-old patient with a clinical history of myocardial infarction, heart failure and global respiratory failure. He had been diagnosed 12 months previously with CMML type 1, for which he had not been treated. He came into contact with the manure when using it as fertiliser.
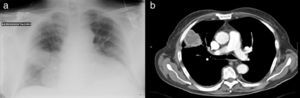
He attended the emergency department due to a decreased level of consciousness, asthenia and drowsiness. Physical examination showed blood pressure 73/47mmHg, heart rate 120beats/min, mild fever and basal oxygen saturation of 86%. He was conscious, prone to bradypsychia and dehydrated. Laboratory tests revealed 59900leukocytes/mm3 with 90% neutrophils and 46000platelets/mm3. Previous tests carried out for regular monitoring of his CMML showed leukocytes 15000/mm3. Chest X-ray showed a rounded high attenuation area in the right hemithorax, with no air bronchogram, measuring 5cm×4cm, on the right parahilar region (Fig. 1a). Blood cultures were drawn and intravenous imipenem treatment was initiated empirically, due to suspected sepsis and pulmonary mass.
Thoracoabdominal computed tomography (CT) was performed (Fig. 1b), showing a heterogeneous mass with marginal spiculation, 5cm in diameter, located in the anterolateral segment of the right upper lobe, with wide pleural contact. Radiologically, the lesion was suggestive of lung neoplasm. Fine needle aspiration was carried out, revealing acute abscessing inflammation associated with a pattern of organizing pneumonia, with no evidence of malignancy. HIV serology was negative. Finally, blood cultures were positive for R. equi.
Patient progress was excellent with imipenem during his hospitalization and following sequential therapy at home with ciprofloxacin and oral rifampicin. Three months later, the pulmonary mass had disappeared and 12 months later the patient remained asymptomatic with periodic check-ups at the haematology clinic.
DiscussionThe first infection caused by R. equi in man was described in 1967. It showed a chronic granulomatous process characterized by aggregates of PAS positive histocytes that contained inclusions known as Michaelis–Gutmann bodies (malacoplakia) and necrotizing abscesses associated with intracellular Gram positive cocci, characteristic of R. equi infection.1 Despite this, malacoplakia is not specific to this infection, as Mycobacterium tuberculosis, Pasteurella multocida and Escherichia coli can cause histologically similar lesions, although not as often in immunocompromised patients.2 The primary infection occurs in the lung in approximately 80% of cases, often presenting cavitated consolidation in the upper lobe.3 It is a rare pathogen in immunocompetent patients, which represent 10%–15% of cases, mainly renal transplant patients.2 In 2010, the first case was reported in which a patient with chronic lymphoid leukaemia developed cavitated pneumonia caused by this microorganism after receiving fluarabin treatment.4
It should be suspected in immunosuppressed patients who present with pneumonia with an insidious clinical course, pulmonary abscess, granulomatous lesions, brain abscess or fever of unknown origin. The radiological differential diagnosis should be made mainly with pneumonia due to Pneumocystis jirovecci or Staphylococcus aureus, central bronchogenic carcinoma and pulmonary tuberculosis. R. equi is usually susceptible to combined antibiotic therapies, which include macrolides, rifampicin, aminoglycosides and imipenem. Two or three antibiotics should always been combined; those with intracellular activity, such as rifampicin or azithromycin, are recommended. With respect to the prognosis, the mortality reaches 50% in HIV patients, 25% in other types of immunosuppression and 11% in immunocompromised patients.5
It is exceptionally observed in immunocompromised patients who do not have HIV, as in our case, where despite not being on active immunosuppressant treatment, the cellular immunosuppression caused by the myelomonocytic leukaemia and contact with the contaminated manure triggered this serious lung infection.
Please cite this article as: Josa Laorden C, Gómez del Valle C, Bucar Barjud M, Amores Arriaga MB, Torralba Cabeza MA, Pérez Calvo JI. Shock séptico por Rhodococcus equi en paciente con leucemia mielomonocítica crónica. Arch Bronconeumol. 2013;49:497–498.