Streptococcus pneumoniae is responsible for several clinical syndromes, such as community-acquired pneumonia, sinusitis, otitis media, and others. The most severe clinical entity caused by this bacterium is undoubtedly invasive pneumococcal disease. Certain factors are known to increase the risk of presenting invasive pneumococcal disease, the most important being smoking and underlying concomitant diseases. This article comprises a consensus document on antipneumococcal vaccination in smokers, drawn up by a Smoking Expert Group from the Spanish Society of Pulmonology and Thoracic Surgery and the Latin American Chest Association.
Streptococcus pneumoniae es causante de diversos cuadros clínicos: neumonía adquirida en la comunidad, sinusitis, otitis media, etc. Sin duda, la forma clínica más grave ocasionada por este germen es la enfermedad neumocócica invasiva. Se sabe que determinados factores, entre los que destaca el consumo de tabaco, y el padecimiento de enfermedades subyacentes concomitantes aumentan el riesgo de padecer estos procesos. Este artículo muestra un documento de consenso sobre vacunación antineumocócica en fumadores que ha sido realizado por un grupo de expertos en tabaquismo de la Sociedad Española de Neumología y Cirugía Torácica y de la Asociación Latinoamericana del Tórax.
Streptococcus pneumoniae (S. pneumoniae) is a Gram-positive coccus, with a capsule containing an antigen that gives it its pathogenicity and virulence. This capsular antigen defines the serotype, and is the basis for vaccine development. More than 92 serotypes of this microorganism have been identified, although not all are pathogenic. It is notable, however, that 23 of them cause 76% of pneumococcal diseases in the world.1 According to World Health Organization (WHO) estimates, pneumococcal disease is responsible for 1.6 million deaths annually, and is the leading cause of vaccine-preventable death.2,3
In Spain, S. pneumoniae was the most frequently identified pathogenic agent in community-acquired pneumonia (CAP) in 2003–2007, being responsible for up to 63.7% of cases. Moreover, during this same period, a total of 75932 deaths due to CAP were recorded in adults aged 50 or older (16.9%).4,5 In a study conducted in Latin America between 1970 and 2008, a wider period than that analyzed in the Spanish study, S. pneumoniae was found to be the most commonly identified CAP-causing pathogen, and was responsible for 35% of cases diagnosed. Furthermore, the mortality in this region due to CAP was higher than in other developed countries: 6% compared to 4%.6
S. pneumoniae causes various clinical conditions, such as CAP, sinusitis, otitis media, and others. The most serious of these is undoubtedly invasive pneumococcal disease (IPD), defined as the presence of S. pneumoniae in blood, cerebrospinal fluid or other normally sterile fluid.7 Certain factors and underlying concomitant diseases are known to increase the risk of IPD. The most important of these underlying diseases are those that cause immune deficiency or impair the local defenses of the target organ, such as chronic respiratory, renal, liver and cardiovascular disease; HIV-positive patients; patients awaiting solid organ transplantation and solid organ and/or hematopoietic stem cell transplant recipients; patients receiving chemotherapy for solid tumors or hematologic neoplasia; those with autoimmune disease, receiving corticosteroids, immunosuppressants or biological products; diabetic patients; patients with cerebrospinal fluid fistulas, cochlear implants; and patients with anatomical or functional asplenia.8 Smoking has also been shown to be a major risk factor for the development of pneumococcal disease.9–14
Up to 4500 toxic substances have been described in tobacco smoke, most of which are pathogenic for humans.9 Many of these substances alter the lung defense mechanisms and cause respiratory bacterial infections, especially pneumococcal infections, to occur more frequently in smokers than in non-smokers.10,11 CAP has been found to develop more often in smokers, and the bacterium most frequently implicated in its etiology is S. pneumoniae.12,13 IPD is also known to be more common in current smokers, passive smokers and in ex-smokers for less than 5 years, than in never-smokers.14 All these data point to smoking as one of the main independent risk factors for the development of CAP and IPD.
In 2012, a group of experts in smoking-related diseases from the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) issued recommendations for pneumococcal vaccination in smokers.15 That same year, the Spanish Society of Preventive Medicine, Public Health and Hygiene published guidelines for pneumococcal vaccination in adults in which it corroborated the recommendations of the SEPAR group.16 These recommendations are also specified in the multidisciplinary guidelines for the management of CAP published in 2013.17 Finally, the Consensus on pneumococcal vaccinations in adults with underlying disease, published in 2013 and endorsed by 16 Spanish scientific societies, also backed SEPAR's recommendations.18
Recently, experts in smoking-related diseases from SEPAR and the Latin American Chest Association (ALAT) discussed the need to publish a consensus document, based on the original SEPAR guidelines, to address the requirement for pneumococcal vaccination in smokers in Spain and Latin America. This working group has been created for various reasons: the high prevalence of smoking and the high rate of pneumococcal diseases diagnosed in these countries (35% in Latin America compared with 63.7% in Spain), the high mortality rate due to CAP, and the need to establish scientific criteria for pneumococcal vaccination in smokers in these countries that share similar social and cultural characteristics.6,13,19–21
In this document, different basic research studies will be presented which support smoking as an important risk factor for the development of pneumococcal disease, and clinical–epidemiological studies conducted in both Spain and Latin America will be reviewed, showing smoking as a major risk factor in these diseases. Finally, risk groups will be defined and a joint proposal for vaccination put forward.
Relationship Between Smoking and Pneumococcal Disease. Review of Basic Research StudiesA higher risk of pneumococcal infection has been described among smokers, fundamentally owing to changes in the epithelium of the bronchial mucosa, increased bacterial adherence, and immune response changes (both innate and adaptive) that occur in this group.22–31 The toxic substances in tobacco smoke produce lesions in the respiratory epithelium that reduce mucociliary clearance. These include: mucous gland hypertrophy, increased goblet cells, loss of cilia, impaired mucus production and altered rheology, as well as disruption of epithelial bronchial cell junctions.22,23 One study also found that human β defensin-2 levels, produced by the bronchial epithelial cells, are lower in smokers and former smokers than in never smokers.24
However, in addition to smoking-induced bronchial epithelial lesions, these toxic substances were also found to alter the number and function of alveolar cells. Various in vivo and in vitro studies have shown that the alveolar fluid of smokers contains a higher number of alveolar macrophages and polymorphonuclear leukocytes, and that the phagocytic capacity of these cells is clearly reduced compared to non-smokers.25–27
Tobacco smoke modifies bacterial adherence, which is key to the development of mucosal or invasive disease, and contributes to the susceptibility of smokers to pneumococcal infection.28 One study showed that exposure to cigarette smoke condensate increased pneumococcal production of biofilm and decreased pneumolysin activity, which could explain the greater colonization and persistence of pneumococcus in smokers.29
Cigarette smoke is also known to affect the immune response. In vitro studies have shown that smokers have a lower cellular immunity response against melanoma cells, and that IgG and IgA production is decreased.30In vivo studies have shown that smoking affects T lymphocyte sub-sets, particularly CD4 populations and the CD4/CD8 ratio.31 In other analyses, tobacco smoke was found to attenuate the inflammatory response of respiratory cells. Tobacco has been shown to inhibit the response of Toll-like receptor-2 (TLR2), nuclear factor κB (NF-κB), CD4 cell proliferation (CD4TL), maturation of dendritic cells, and opsonization capacity.32–36 The findings of these in vivo and in vitro studies, therefore, clearly suggest that cigarette smoke alters the immune response of the respiratory cells.
Table 1 summarizes the main conclusions of basic research studies analyzing smoking-induced changes in the respiratory tract, and how these lead to a higher incidence of infection (particularly pneumococcus) and infection-induced mortality in smokers.
Changes in the Respiratory Tract Caused by Smoking.
| 1.- Mucociliary epithelial changes |
| - Loss of cilia |
| - Mucous gland hypertrophy |
| - Increased goblet cells |
| - Impaired mucus production |
| - Altered mucus rheology |
| - Disruption of bronchial epithelial cell junctions |
| - Reduced production of human β defensin-2 |
| 2.- Increased bacterial adherence |
| - Decreased pneumolysin production |
| - Increased biofilm production |
| 3.- Changes in the immune response |
| - Reduced phagocytosis by alveolar macrophages and polymorphonuclear leukocytes |
| - Reduced cytokine production |
| - Reduced immunoglobulin production |
| - Altered lymphocyte sub-sets |
Various clinical–epidemiological studies have found that smoking is an independent risk factor for the development of CAP and IPD.
In a population-based, case-control study conducted in Spain by Almirall et al., in which 1336 cases of CAP were identified out of a population of 859033 subjects, multivariate analysis revealed that smoking was a risk factor for developing this disease: OR: 1.48 (1.14–1.86).37 Another study by the same group also found a dose/response relationship between smoking and the likelihood of developing CAP: the longer the history of smoking, the greater the number of cigarettes smoked and the number of pack-years, the higher the risk of developing CAP. After smoking cessation, the probability of developing CAP decreased by 50% after 5 years of abstinence.38 This relationship between CAP and smoking has been found in numerous studies. Thus, Torres et al., in a literature review of 60 publications, found that smoking is a major risk factor for CAP, OR: 1.81 (1.53–2.15).39
Other studies have also found that smoking is an independent risk factor for severe pneumococcal CAP, with an OR of 2.11 (1.02–4.34, P=.04) for septic shock.40,41 Furthermore, in the HIV-positive population, in the era of combined anti-retroviral treatment, smoking was described in various studies as the main risk factor for developing CAP.42,43 One epidemiological study showed that smoking is an independent risk factor for mortality in bacteremic CAP due to S. pneumoniae.44 A recent Spanish study investigated the effect of smoking on mortality due to pneumococcal CAP45 in 4288 patients hospitalized for CAP, of which 892 had pneumococcal CAP. Current smoking was an independent risk factor for increasing 30-day mortality in subjects with pneumococcal CAP (OR 5.0 (1.8–13.5; P=.001), after adjusting for various confounding factors (age, liver disease, sepsis, etc.).45
However, it is not only active smoking that has been linked to the development of CAP; passive smoking has also been shown to be a risk factor. A population-based, case-control study found that passive smoking was a major risk factor for the development of pneumococcal bacteremia in immunocompetent subjects.14
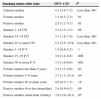
IPD is another condition in which smoking has been shown to be a major risk factor. According to a Spanish prospective, multicenter, hospital-based surveillance study (ODIN study) conducted from 2010 to 2012, in which a total of 436 patients were analyzed (both immunosuppressed and immunocompetent), smoking was found to be the main risk factor.46 It was also shown to be the main independent risk factor for the development of IPD in immunocompetent adults in a population-based study.14 The authors of this study analyzed all immunocompetent subjects with IPD in various American and Canadian cities. A total of 228 subjects were identified and a total of 301 were used as controls. The authors found that IPD was significantly associated with smoking: OR, 4.1 (2.4–7.3). Furthermore, there was a positive dose/response relationship, not only with the number of pack-years, but also with time since quitting (Table 2).14 The attributable risk for passive smoking was 17%.14 One of the most interesting findings of this study was that even in patients with only a one pack-year smoking history, the risk of developing IPD could have already doubled, and that the risk in a former smoker did not fall to that of a never-smoker until at least 10 years after they had quit.14 Another population-based study with similar characteristics also found that smoking was a significant risk factor for developing IPD,47 with an OR of 2.6 in smokers aged between 24 and 64 years, and an OR of 2.2 in smokers aged over 65 years. The attributable risk was 31% in the first group and 13% in the second.47
Relationship Between Active and Passive Smoking and the Risk of Developing IPD.
| Smoking status odds ratio | (95% CI)a | P |
|---|---|---|
| Current smoker | 4.1 (2.4–7.3) | Less than .001 |
| Former smoker | 1.1 (0.5–2.2) | .91 |
| Passive smoker | 2.5 (1.2–5.1) | .01 |
| Smoker 1–14 CD | 2.3 (1.3–4.3) | .06 |
| Smoker 15–24 CD | 3.7 (1.8–7.8) | Less than .001 |
| Smoker 25 or more CD | 5.5 (2.5–12.9) | Less than .001 |
| Smoker 1–14 P-Y | 1.5 (0.9–2.5) | .1 |
| Smoker 15–29 P-Y | 3.0 (1.4–6.6) | .006 |
| Smoker 30 or more P-Y | 3.2 (1.6–6.9) | .002 |
| Former smoker less than 5 years | 3.5 (1.3–9.8) | .02 |
| Former smoker 5–9 years | 3.7 (1.1–13.2) | .04 |
| Former smoker 10 or more years | 0.6 (0.2–1.3) | .18 |
| Passive smoker (4 or less hours/day) | 2.4 (0.9–6.3) | .08 |
| Passive smoker (more than 4h/day) | 3.9 (1.0–16.1) | .05 |
CD: cigarettes per day; P-Y: pack years.
In view of the findings of these studies, it is evident that smoking is a very significant risk factor for the development of pneumococcal disease in its clinical forms of CAP and IPD. Undoubtedly, the best advice we should give to a smoker to reduce their risk of pneumococcal disease is to quit smoking. This could reduce the risk of CAP by 50% after 5 years and reduce the incidence of IPD by 14% with every non-smoking year, bringing their level of risk after 10 years to that of a never smoker.14,38
This working group of experts in smoking-related diseases from SEPAR and ALAT also agreed that pneumococcal vaccination should be recommended in the following groups of smokers:
- •
Group 1. – Smokers with no comorbidities and a history of one or more pack-years.
- •
Group 2. – All smokers, regardless of their intensity and/or history of tobacco use, who have the following conditions:
- •
Group 2.A. – Smokers with primary immune deficiencies.
- •
Group 2.B. – Smokers with immune deficiencies secondary to:
- •
Awaiting solid organ transplant or transplant recipients (6 months post-transplant).
- •
Chemotherapy or radiotherapy: 15 days before initiating treatment or 3 months after discontinuation.
- •
Long-term corticosteroid treatment.
- •
Chronic renal disease.
- •
HIV-positive patients.
- •
Patients with hematopoietic stem cell transplants.
- •
Patients with hematological malignancy.
- •
Patients with autoimmune disease or receiving immunosuppressants or biological products.
- •
Anatomical or functional asplenia.
- •
- •
Group 2.C. –Smokers with:
- •
Chronic liver disease.
- •
Chronic lung disease.
- •
Chronic heart diseases.
- •
Diabetes.
- •
Cerebrospinal fluid fistulas.
- •
Cochlear implants.
- •
Chronic alcoholism.
- •
- •
Group 3. – Former smokers of at least one pack-year who have been abstinent for less than 10 years.
The expert group would like to state that some countries may encounter difficulties in implementing vaccination in some adults who are not covered by national health insurance schemes. This is an added difficulty for extending vaccination to these risk groups and, certainly, a barrier for implementation.48 Nevertheless, a literature review that analyzed a group of economic evaluation studies of 23-valent pneumococcal polysaccaride vaccine (PPSV23) in adults found that immunization with this vaccine was cost-effective, and in some cases was a cost-saving strategy for the prevention of IPD.49
In August 2014, the Advisory Committee on Immunization Practices analyzed the preliminary results of the CAPiTA study and evaluated the scientific evidence supporting the use of the 13-valent pneumococcal conjugate vaccine (PCV13) in adults using the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) system. As a result, the evidence was classed as Level 2 (moderate level of evidence), and the recommendation was awarded Category A status.50
Guidelines for Vaccine AdministrationTaking into account these recommendations and those specified by other groups in other consensus documents, the SEPAR/ALAT expert group have agreed to recommend the prioritization of PCV13 with two vaccination guidelines: one for smokers not previously vaccinated with PPSV23, and another for those who have been vaccinated with this formulation.15–18,50–52
- 1.
Smokers not previously vaccinated
In this case, it is recommended that subjects from all groups receive at least one dose of PCV13, and that subjects in groups 2.A and 2.B receive one dose of PPSV23 at least 2 months after having received the PCV13 dose.
- 2.
Smokers previously vaccinated with PPSV23
In this case, it is recommended that subjects from all groups receive at least one dose of PCV13, one year after having received the PPSV23 dose. Moreover, subjects in groups 2.A and 2.B should receive a new dose of PPSV23 at least two months after having received the PVC13 dose, if the first PPSV23 dose was five or more years previously.
This study was funded by an unconditional grant from Pfizer to the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) and the Latin American Chest Association (ALAT).
Conflict of InterestsAuthors Carlos Andrés Jiménez Ruiz, Daniel Buljubasich, Raúl Sánsores, Juan Antonio Riesco Miranda, Alfredo Guerreros Benavides, Susana Luhning, José Miguel Chatkin, Gustavo Zabert, José Ignacio de Granda Orive and Segismundo Solano Reina have no conflicts of interest to declare. Dr. Alejandro Casas is a member of the Boehringer and Novartis Advisory boards, and speaker for Boehringer, Novartis, MSD and GSK. Dr. Pilar de Lucas Ramos has received a research grant from Almirall, is a member of the Almirall and Takeda advisory boards, and participates in Boehringer, Pfizer and Novartis meetings.
Please cite this article as: Jiménez Ruiz CA, Buljubasich D, Sansores R, Riesco Miranda JA, Guerreros Benavides A, Luhning S, et al. Documento de consenso SEPAR-ALAT sobre vacunación antineumocócica en fumadores. Arch Bronconeumol. 2015;51:350–354.