The aim of our work is to promote awareness about the development of sarcoidosis after anti-neoplastic therapy in order to avoid diagnostic errors with FDG-PET/CT findings. We report the observation of three women with breast, cervix and stomach treated cancers who developed a sarcoidosis after the end of anti-neoplastic therapy.
The utility of FDG-PET/CT is in pinpointing the candidates’ organs for diagnostic biopsy and not for distinguishing between the malignancy and granulomatous or inflammatory diseases.
El objetivo de este trabajo es concienciar sobre el desarrollo de sarcoidosis tras el tratamiento antineoplásico para evitar errores de diagnóstico con los estudios de FDG-PET/CT. Se presentan los casos de 3 mujeres tratados de cáncer de mama, cuello uterino y estómago, que desarrollaron sarcoidosis al finalizar el tratamiento antineoplásico.
La utilidad del FDG-PET/CT está en la localización de órganos candidatos a biopsia diagnóstica, pero no sirve para distinguir un tumor maligno y lesiones inflamatorias o granulomatosas.
Sarcoidosis is a multisystem inflammatory disease of unknown etiology. It is difficult to make a differential diagnosis in patients with present or previous malignancies.
The aim of this paper is to raise awareness about the development of this disease after cancer treatment to avoid misdiagnosis with FDG-PET/CT studies. The goal is not to make any assessment of the prevalence of sarcoidosis or sarcoid reactions in patients who have undergone cancer treatment.
Unfortunately, endobronchial ultrasound (EBUS) is not yet developed in our country. We conducted over 340 FDG-PET/CT scans for follow-up after cancer treatment. Sarcoidosis was diagnosed in the mediastinum of 3 patients (0.9%) in accordance to their clinical and pathological data.
Case 1On July 2009, a 48-year-old woman with no medical history presented with right breast tumor (1cm in diameter) of the superior external quadrant. The patient underwent right external superior quadrantectomy with axillary lymphadenectomy. The histological examination showed an infiltrating lobular carcinoma with metastases in all 8 distant nodes.
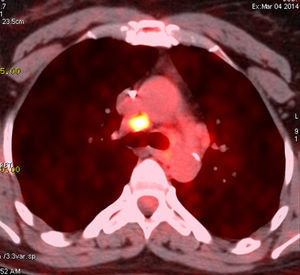
The patient received postoperative radiotherapy (45Gy) and hormonal therapy (tamoxifen) for 12 months. Two years later, new right axillary lymph node metastases were discovered and removed. One year later, chest CT showed in the mediastinum the presence of multiple lymph nodes with positive uptake value in the FDG PET scan (Fig. 1). The bronchoscopy was normal. Since standard uptake values (SUV) were low, a second FDG PET was performed 3 months later, showing stable lymph node growth. Mediastinoscopic biopsy of lymph nodes was performed, and it revealed non-caseating giant cells granulomas, consistent with sarcoidosis. The patient received corticoids, with good outcome.
Case 2In March 2009, a 47-year-old woman diabetic under treatment with insulin therapy for 3 years presented with epidermoid carcinoma of the cervix with multiple abdominal lymph nodes. She received chemotherapy (2 cycles of combination bleomycin, etoposide and cisplatin, and then 2 cycles of combination etoposide, carboplatin and ifosfamide), followed by a hysterectomy and abdominal and pelvic lymph node removal. Three years after completion of the therapy (December 2012) the patient reported progressive dyspnea. Bronchoscopy was normal; an FDG-PET/CT scan showed mediastinal and hilar nodes. She was therefore referred to our department for mediastinoscopy on suspicion of malignant recurrence. Following mediastinoscopy, lymph node biopsy was performed, which showed lymph node sarcoidosis, with no malignancy.
Case 3A 59-year-old women with no medical history was referred to our department because of chronic vomiting related to a gastric pylorus mass. Analysis of biopsy specimens indicated stomach carcinoma. After gastrectomy in February 2011, histology showed tubular adenocarcinoma. She underwent 4 cycles of chemotherapy with carboplatin over 13 weeks (until June 2011). The clinical signs such as vomiting resolved gradually after surgery and chemotherapy, and the patient's condition was managed favorably. She recently (30 months after surgery) presented with an unexplained chronic cough; a chest CT scan showed multiple lymph nodes in the Barety's space and right paratracheal area. The bronchoscopy was normal. The most likely diagnosis was lymph node metastasis; however, histology of tissue samples obtained with mediastinoscopy showed sarcoidosis.
The clinical data are summarized in Table 1.
Clinical and Therapeutic Data of Our Three Cases.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age and sex | 48 years. Female | 47 years. Female | 59 years. Female |
| Medical history | None | Diabetes. Under insulin therapy | None |
| Cancer | Local breast lobular carcinoma | Epidermoid carcinoma of cervix | Tubular adenocarcinoma of the stomach (stage 1) |
| Anti-neoplastic therapy | Surgery (quadrantectomy and axillary node removal) | Chemotherapy (4 cycles) | Gastrectomy 4/5 |
| Radiotherapy+hormonal therapy: tamoxifen | Hysterectomy and abdominal and pelvic lymph nodes removal | Chemotherapy (4 cycles): carboplatin | |
| Key dates | July 2009: breast surgery | March 2009: chemotherapy | February 2009: surgery |
| June 2012: surgery for axillary lymph nodes | June 2009: surgery | June 2009: end of chemotherapy | |
| July 201: positive PET/CT | December 2012: positive PET/CT | August 2013: positive uptake in PET/CT | |
| Disease-free interval | 13 months | 3 years 6 months | 4 years 2 months |
| Chest PET/CT: mediastinal nodes | SUVmax at 3.6 | SUVmax at 5.1 | SUVmax at 8.7 |
| Biopsy | Cervical axial mediastinoscopy | ||
| Pathology | Sarcoidosis | ||
| Treatment | Corticoids | None | Corticoids |
| Outcome | Good (mediastinal lymph node recurrence) | Stable | Good (mediastinal lymph node recurrence) |
Even with similar histological features, granulomas in sarcoid reactions are B-cell negative whereas those in sarcoidosis are B-cell positive.1
The relationship between anti-neoplastic treatment and sarcoidosis is controversial.2 Some authors believe that it is linked to the type of malignancy, genetic predisposition, and anti-neoplastic therapy that can trigger onset of sarcoidosis.
Differential diagnosis includes all causes of granulomatosis.
Repeat FDG-PET can be used to assess the activity of sarcoidosis and its response to therapy.3 Even when sarcoidosis is confirmed, we repeat PET/CT to eliminate a concomitant lymph node metastasis. Generally, symmetrical hilar FDG uptake may be related to a benign cause.4
Spontaneous remission of sarcoidosis occurs in 60% of patients,5 and reduced FDG uptake could be a marker to rule out recurrent malignancy. However, a significant reduction in FDG uptake is only noticeable over time (6 months), and the repeated use of PET/CT is costly.
In conclusion, sarcoidosis is an FDG avid lesion. In our opinion, PET/CT is useful for targeting organs for diagnostic biopsy, but does not distinguish between recurrent malignancy and granulomatosis.
Conflict of InterestThe authors have no conflict of interest to declare.
Please cite this article as: El Hammoumi M, El Marjany M, Moussaoui D, Doudouh A, Mansouri H, Kabiri EH. Sarcoidosis mediastínica imitando recidiva de cáncer linfáticotras tratamiento antineoplásico. Arch Bronconeumol. 2015;51:e33–e35.